J Sci Discov (2018); 2(1):jsd18001; DOI:10.24262/jsd.2.1.18001; Received October 28th, 2017, Revised January 01st, 2018, Accepted January 18th, 2018, Published January 25th, 2018.
Large Intestinal Lymphangiectasia Polyp, a benign condition with clinical consequences
Mohanad A. Albayyaa1, Omar N. Saab1, Harith Alataby1, Amna Altkrit1, Nisar Ahmed1,*
1Department of Gastroenterology, Park Plaza Hospital, Houston, TX, 77004
* Correspondence: Nisar Ahmed, M.D. F.A.C.G, Chief of Gastroenterology, Park Plaza Hospital, Houston, Tx 77004, USA.E-mail: nisarahmedmd@yahoo.com
Abstract
Intestinal Lymphangiectasia is an important condition of gastrointestinal tract that endoscopic finding shows polyp. Only a few cases had been reported. Sometimes it was found to be associated with telangiectasia. It is benign condition and sometimes shares similar symptoms of malignancies that needs to be differentiated from other serious conditions like lymphoma.
Keywords: Intestinal Lymphangiectasia, Polyp, Benign, Malignancy
Introduction
Intestinal lymphangiectasia is a relatively rare condition of gastrointestinal tract that is seen as pathological dilation of lymph, blood vessels and main cause of protein losing enteropathy.[1] It is classified into two groups: primary type, which has no particular causes, and secondary type, which is associated with marked inflammation. It is characterized by hypoproteinaemia, oedema and lymphocytopenia.[2]
Case Report
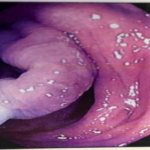
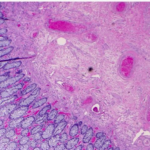
A 60 years old Hispanic female was referred for colon cancer screening. She had never had a colonoscopy. She was in good health and gave no history of change in her bowel habits, abdominal pain, or rectal bleeding. On colonoscopy she was found to have a large unusual looking polyp as shown in Figure-1. Biopsies of the polyp showed that it consisted of lymphangiectasia, and telangiectasia as shown in Figure-2.
Figure-1: Large Intestinal polyp by colonoscopy
Figure-2: Histological examination of Intestinal Lymphagectesia showed dilatation of the lymphatic in the mucosa, submucosa of the bowel and blood vessels dilatation as shows by arrows.
Discussion
The Primary intestinal Lymphangectesia occurs in children and adults due to congenital deformity of bowel lymphatic system and the secondary one is more frequently in adults, the patient may be asymptomatic or manifest an elevated lymphatic pressure as in lymphoma, systemic lupus erythematosus, inflammatory bowel disease, malignancies, constructive pericarditis and cardiac disease.[2,3]
Intestinal Lymphangiectasia was first described in 1961 by Waldmann and characterized by dilation of intestinal mucosa, submucosal and subserosal intestinal lymphatics leading to obstruction, rupture and leak of lymph fluid in the bowel lumen that cause lymphopenia, hypogammaglobulinemia and albuminemia.[3] The diagnosis can be made by clinical manifestations including fatigue, chronic diarrhea, abdominal pain, nausea, bilateral lower limb oedema, ascites and sometimes with recurrent gastrointestinal bleeding, then the definitive diagnosis requires endoscopy and biopsy.[4] The endoscopic findings are scattered white plaques covering the mucosa but it may be normal and in such cases video capsule endoscopy and double balloon enteroscopy assisted biopsy to make the diagnosis.[3] The diagnosis of intestinal lymphangiectesia is established by histology of the grossly dilated lymphatic’s seen in lamina propria of the small bowel (Duodenum, Jejunum and Ileum), the villi is distorted and enlarged.[5] There are some syndromes linked with Intestinal Lymphangiectesia like Turner, Von Ricklinghaeson, Noonan, Hennkam and yellow nail.[3] The immunological findings of intestinal lymphangectasia are low CD4 T cells, skin allergy, reduced immunoglobulin levels (IgA, IgG, IgM), lymphocytopenia and graft rejection.[4]
There had been few similar cases reported regarding asymptomatic Intestinal Lymphangiectasia, and it was shown by dilatation of intestinal lymphatics leading to obstruction, rupture and leak of lymph into the bowel lumen. It can be confused or misdiagnosed with secondary malignancies like lymphoma, systemic lupus erythematosus, and patients treated with chemotherapy and radiotherapy.[7]
Conclusion
Intestinal Lymphangiectasia, so far, is usually a benign
condition with clinical consequences. Sometimes, it’s presented with symptoms and very rare discovered by screening (asymptomatic). However, this does not mean to overlook this disorder, it is very important to exclude other serious conditions especially lymphoma and secondary malignancies.
Conflict of interest
None
Acknowledgments
None
References
1. Waldmann TA, Steinfeld JL, Dutcher TF, Davidson JD, Gordon RS Jr. The role of the gastrointestinal system in “idiopathic hypoproteinemia”. Gastroenterology 1961; 41:197-207
2. Takenaka H, Ohmiya N, Hirooka Y et al. Endoscopic and Imaging Findings in Protein-losing Enteropathy. J Clin Gastroenterol 2011.
3. Vignes S, Bellanger J. Primary intestinal lymphangiectasia (Waldmann’s disease).Orphanet Rare Dis 2008; 3: 5.
4. Lee WS, Boey MCC, Goh TAY, Chang KW, Iyngkaran N. Intestinal lymphangiectasia – A report of three Chinese children in Malaysia .Singapore Med J 1998; 39: 418-421.
5. Tift WL, Lloyd JK. Intestinal lymphangiectasia long term results with MCT diet. Arch Dis Child 1975; 50: 269-276.
6. Heresbach D, Raoul JL, Genetet N, Noret P, Siproudhis L, Ramee MP, et al. Immunological study in primary intestinal lymphangiectasia. Digestion 1994; 55: 59-64.
7. Tift WL, Lloyd JK: Intestinal lymphangiectasia: Long-term results with MCT diet. Arch Dis Child 50:269–275, 1975.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/