J Sci Discov (2017); 1(1):jsd17005; DOI:10.24262/jsd.1.1.17005; Received May 11th, Accepted May 21st, Published May 21st.
Clinical Buddhist Chaplaincy Training Program: History of the Development of Taiwan’s Clinical Buddhism
Rong-Chi Chen
1En Chu Kong Hospital,Sanhsia District,New Taipei City, 23702, Taiwan.
* Correspondence: Rong-Chi Chen,MD,PhD,FANA. En Chu Kong Hospital,Sanhsia District,New Taipei City, 23702, Taiwan. Email: rongchichen@gmail.com.
Abstract
Morden hospice palliative care was introduced into Taiwan in 1990. Buddhist Lotus Hospice Care Foundation(LHCF) was organized in 1994 to join the hospice movement. In order to invite Buddhist chaplains to join the care of hospice patients, LHCF started to establish Clinical Buddhist Chaplaincy (CBC) Training Program at the palliative unit of the National Taiwan University Hospital in 1998. It has succeeded complete training of 63 chaplains. 33 of them now served in 44 hospice units in Taiwan. The participation of the certified Clinical Buddhist Chanlains(CBCs) in the hospice care has remarkably improved the quality of spiritual care for the terminal patients. Being the first in the hospice history and also Buddhist history, this CBC training system has spreaded from Taiwan to Japan.
Keywords: Hospice palliative care, clinical Buddhism, clinical chaplaincy, clinical Buddhist chaplain (CBC), clinical monastic, Hospice palliative care act, Patient self determination act, Natural death act, good death, peaceful death, dignified death
Introduction
Modern hospice palliative care organization was started by Dr. Dame Cicely Saunders at the St. Christopher’s Hospice in London in 1967.[1] This humane form of holistic health care has gradually spread around the world, reaching Taiwan in 1990 at the Christian Mackay Memorial Hospital in Tamsui, Taipei County in 1990 [2]. The second hospice ward was established in 1994 at the Catholic Cardinal Tien Hospital in Hsindian, Taipei County. In 1994 the author was invited by the Christian Hospice Foundation of Taiwan to visit a few leading hospices in Japan to learn more about the management [3]. In 1995 the author opened a palliative unit at the National Taiwan University Hospital (NTUH) in Taipei City, the first in the public government-owned hospital and university hospital[3]. It added the momentum of spreading of hospice palliative care over Taiwan.
Development of Hospice Palliative Care in Taiwan
With the cooperation of the 3 major religious organizations, the Christian Hospice Foundation of Taiwan [4], the Catholic Sanipax Socio-Medical Service & Education Foundation [5], and the Buddhist Lotus Hospice Care Foundation(LHCF)[6], together with many non-governmental organizations (NGOs) and the governmental support, the hopspice palliative care movement flourished in Taiwan [7]. With a population of 23 millions, and a territory of 36,000 Km2, we now have 62 hospice wards in general hospitals, 101 hospice home care teams, 200 hospice community care teams. Hopsice Palliative Care Act (a Natural Death Act) was established in 2000 [8] and Patient Self Determination Act was promulgated in 2016 [9]. Taiwan was twice ranked the first in Asian countries in the quality of end-of-life care by the Lien Foundation [10,11].
The Hospice Palliative Care Act gives our people the right to choose do no resuscitation (DNR) at the terminal stage of life [8]. According to the Patient Self Determination Act, “the patient can ask for withholding or withdrawal of the life sustaining treatments if he/she is 1. A terminal patient, 2. In the irreversible comatous state, 3. In the persistent vegetative state, 4. In the severe dementia state, 5. The patient is in intolerable pain, an incurable disease without adequate solution under the current medical standard.” These life-sustaining treatments include cardiopulmonary resuscitation (CPR), artificial ventilation, mechanical life sustaining system (such as ECMO), blood substitutes, chemotherapy, dialysis, antibiotics for fatal infections, artificial nutrition and artificial liquid feeding, etc. [9,12].
Need for Clinical Buddhist Chaplains in the Spiritual Care
Shortly after the beginning of the Palliative Ward at National Taiwan University Hospital in 1995, a Buddhist nun and then a monk volunteered to join the team to provide spiritual care of hospice patients. However, without the proper preparation of knowledge about the medical conditions of the patients they both failed and quit.
Although spirituality doesn’t necessarily pertain to religion, if religious representatives can become fully involved, the spiritual care that they could provide would be much more effective. Christian denominations have had specific training for chaplains to serve in hospitals and other places yet Buddhist groups have not. As 70-80% of Taiwanese are Buddhist, it would be good to invite some enthusiastic monks and nuns to begin such training. [13,14]
Clinical Buddhist Chaplaincy Training Program
Since 1998, the Buddhist Lotus Hospice Care Foundation (LHCF) began to cooperate with the Palliative Unit of the National Taiwan University Hospital to start the Clinical Buddhist Chaplaincy (CBC) Training Program. [13,14] The program was funded by the LHCF.
Prof. CY Chen, the chairman of the Family Medicine Department of the National University Hospital [15] and Ven. Huimin, chancellor of the Dharma Drum Mountain Institute of Liberal Arts [16] were invited to preside over the CBC Training Program. “Clinical Buddhist Chaplain” refers to the Buddhist chaplain who has been trained and takes up front-line duties in the hospice and palliative care medical team, offering care to patients in the body, mind, social and spiritual aspects; who is also one of the core members of the hospice and palliative care medical team.”[6,17]
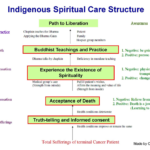
Figure 1. Spiritual Care Structure. Quoted from Chen CY. [15,18] with permission and minor modification.
The content of the CBC Training Program consists of 62.5 hours of classroom courses and 80 hours of Internship bedside practice in the hospice ward (from Monday to Friday, 8 hours per day for 2 weeks). The classroom curriculum includes introductory history of hospice palliative care, medical conditions of terminal patients suffering from cancer or major organ failures, psychosocial and spiritual need of terminal patients, ethical and legal problems, grief consoling of family members, preparation for discharge from hospital, application of Buddhist doctrines in hospice care, clinical application of life and death education, etc. After finishing 62.5-hour classroom course, and 80-hour intership, test will be given. Those passed the test, can enter bedside Residency training course for 600 hours in 15 weeks in hospice ward. After passing the final test they were issued the Certificate of CBC by LHCF. Then they are introduced to hospice service most convenient for them to attend to become a spiritual care member of the hospice team.
Prof. CY Chen designed an Indigenous Spiritual Care Structure to summarize the core issue of CBC in spiritual care. [15,18] (Fig. 1). Following The Four Noble Truths of Buddha’s teaching: Sufferings, Causation (of sufferings), Cessation (of sufferings) and Path (to liberation or to Pure Land of Paradise), he tried to fit into the patient’s conditions: truth telling, acceptance of death, experience the existence of spirituality, and through Buddhist teachings and practice to the final path of liberation.
Ven. Huimin claimed that “The spiritual stage could be lifted in palliative medical care but the results were more obvious with the guidance of the Buddhist chaplain. When terminal cancer patients are faced with worsening symptoms and approaching death, spiritual care can significantly improve the quality of life.” [16]
Up to May 2017, there were 63 completed the training (including 2 Catholic nuns), 33 CBCs serving in 44 hospices in Taiwan. (Fig. 2) Many others engaged in community services. They are required to attend continual education regularly. A senior teacher will travel to visit each hospice with CBC once a year to encourage them, listen to their need and extend help from LHCF if needed [19]. A Taiwan Association of Clinical Buddhist Studies was established in 2007 to strengthen the team spirit of the CBCs [20]. This Association is also active to participate the community hospice care activities of Taipei City Hospitals.
There are thousand ways of dharma-practice in Buddhism. The most commonly used practices in hospice care by the CBCs consist of the following: 1. Practicing all righteousness, 2.Take refuge in theTriple Gems, 3.Recitation of Buddha’s name, 4.Practice on counting the breath, 5.Repentance, 6.End-of-life Dharma speech and reciting Buddha’s name to dying patients, 6.Meditation (dhyana). After nearly 20 years history of participating in the clinical work in hospices, 2 books collecting many heart-touching stories of how peaceful death was achieved by the spiritual care of the CBCs were published, i.e. Stethoscope and Rosary (240 pages), and The Mysteries of Life and Death (319 pages).[21,22] The strong impact of these books was reflected by the good sale and need of reprintings in short intervals.
Fig 2. Distribution of Clinical Buddhist Chaplains Serving in Taiwan’s Hospices
Spreading of CBC Training Program Abroad
In the trainees there were Catholic nuns, Japanese Buddhist monastics, nuns from Malaysia and Singapore. The training program has spreaded to Japan in 2013
[14,23]. A nun from Malaysia completed the CBC training course and returned to Malaysia to participate in the hospice care. Hope this will further expand to other nations with large proportion of Budddhist followers in the population.
“In one’s final moments, quality of life may be more important than the mere prolongation of existence. Physicians who respect patients’ wishes and provide hospice palliative care, can foster a peaceful and dignified departure from life, although the benefits that this provides may not be easily determined empirically. Filial duty and love should find its expression in being with the family member at the end of his or her life, and in encouraging acceptance of disease, quiet life in his last days and peaceful passing. Where it is unavoidable, the death of a patient is not a medical failure. Not being able to facilitate a peaceful and dignified demise is, however.” [24] Life is the best gift and good death is the most beautiful blessing. [6]
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
None
References
1. St. Christopher’s Hospice, 1976. http://www.stchristophers.org.uk/
2. Lai YL, Su WH. Palliative medicine and the hospice movement in Taiwan. Support Care Cancer. 1997; 5(5):348-50.
https://www.ncbi.nlm.nih.gov/pubmed/9322344
3. Chen RC. The spirit of humanism in terminal care. Open Area Studies J, 2009; 2: 7-11.
http://benthamopen.com/contents/pdf/TOARSJ/TOARSJ-2-7.pdf
4. Hospice Foundation of Taiwan, 1990 http://www.hospice.org.tw/
5. Catholic Sanipax Socio-Medical Service & Education Foundation, 1993. http://www.kungtai.org.tw/
6. Buddhist Lotus Hospice Care Foundation,1994. http://www.lotus.org.tw/introduction.pdf http://www.lotus.org.tw/
7.Hospice Foundation of Taiwan. Hospice and palliative care in Taiwan,2015. http://hospice.org.tw/2009/english/index.php
8. Hospice Palliative Care Act. (2000) http://law.moj.gov.tw/Eng/LawClass/LawAll.aspx?PCode=L0020066
9. Patient Self-Determination Act. (2016)
http://law.moj.gov.tw/Law/LawSearchResult.aspx?p=A&k1=%e7%97%85%e4%ba%ba%e8%87%aa%e4%b8%bb%e6%ac%8a%e5%88%a9%e6%b3%95&t=E1F1A1A2&TPage=1
10. Lien Foundation.(2010). The quality of death, Ranking end-of-life care across the world. Economist Intelligence Unit, The Economist. 1-36. http://www.eiu.com/sponsor/lienfoundation/qualityofdeath
11. Lien Foundation.(2015). The 2015 quality of death index, Ranking palliative care across the world. Economist Intelligence Unit, The Economist.1-71. http://www.lienfoundation.org/sites/default/files/2015%20Quality%20of%20Death%20Report.pdf
12.Chen RC. Promotion of advance care planning in Taiwan. J Sci Discov (2017); 1(1):jsd17002; DOI:10.24262/jsd.1.1.17002.
http://www.e-discoverypublication.com/short-communication/
13. Buddhist Lotus Hospice Care Foundation . The Lotus Blossom: The Clinical Buddhist Chaplaincy Training Program in Hospital Sites, DVD., 2009..
14. Watts JS, Tomatsu Y. The Development of indigenous hospice care and clinical Buddhism in Taiwan. in Watts JS, Tomatsu Y. (eds). Buddhist Care for the Dying and Bereaved. Boston: Wisdom Publications, 2012.
http://jneb.jp/english/wp-content/uploads/2013/10/Indigenous-Hospice-Care-and-Clinical-Buddhism-in-Taiwan.pdf
15. Chen CY. Clinical Buddhist chaplain based spiritual care in Taiwan. Taiwan J Hospice Pall Care. 17(3): 300-309, 2012.
http://www.lotus.org.tw/doc/(2)_Document.pdf
16. Huimin Bhikshu . The role of mindfulness in hospice palliative care in Taiwan. Taiwan J Hospice Pall Care 17(2):200-206, 2012.
http://www.lotus.org.tw/doc/(1)_Document.pdf
17. Lotus Hospice Care Foundation. Time for hospice care since 1994. http://www.lotus.org.tw/introduction.pdf
18. Chen CY. The spiritual care model for end-stage cancer patients in Taiwan. Formosan J Med 8(5): 664-671, 2004.
http://ntur.lib.ntu.edu.tw/bitstream/246246/173067/1/73.pdf http://www.lotus.org.tw/doc/%E6%9C%AC%E5%9C%9F%E5%8C%96%E9%9D%88%E6%80%A7%E7%85%A7%E9%A1%A7%E6%9E%B6%E6%A7%8B%EF%BC%88%E4%B8%AD%E3%80%81%E8%8B%B1%EF%BC%89.pdf
19 . Hui-zhe Bhikkhuni . The path to hospices. LHCF Bimonthly. 124: 8-12, 2014.
http://www.lotus.org.tw/upload/124%E3%80%90%E5%A1%B5%E7%9B%A1%E5%85%89%E7%94%9F%E3%80%91%E5%AE%89%E5%AF%A7%E8%A1%8C%E8%85%B3%EF%BC%8F%E9%87%8B%E6%85%A7%E5%93%B2.pdf
20. Taiwan Association of Clinical Buddhist Studies. 2017. http://foundations.olc.tw/foundations/view/554afc22-0ab8-4cf0-b85e-0d1cacb5b862
21. Yao CA(ed). Stethoscope and Rosary. Taipei: Locus Publishing. 2012. http://www.books.com.tw/products/0010531782
22. Huimin Bhikshu, Der-Chia Bhikkhuni, Tsung-Tueng Bhikkhuni . (eds). The Mysteries of Life and Death. Taipei: San Ying Publishing. 2016.
http://www.books.com.tw/products/0010734961
23. Chen RC. Spreading of Clinical Buddhist Chaplaincy training system to Japan. Health E World 2015, May.
http://www.health-world.com.tw/main/home/tw/thishealth_edit.php?id=65&page=29
24. Chen RC. Medical personnel should actively promote the concept of terminal DNR. Tzu Chi Med J 2006; 18:155-157.
https://app.tzuchi.com.tw/file/tcmjd/95-2/18-2-155-157.pdf
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/