J Med Discov (2024); 9(1): jmd24015; DOI:10.24262/jmd.9.1.24015; Received December 22nd, 2023, Revised Februray 10th, 2024, Accepted Februray 22nd, 2024, Published March 8th, 2024.
Plt/HDL is an independent predictor of long-term outcome in patients with ESCC
Shumin Cao1,2, Shuangqing Chen3,4, Shuang Zhang1,4, Qingxin Zhao1,4, Jing Zhao*1
1Department of Oncology,Hebei General Hospital, Shijiazhuang 050057, China
2Graduate School,Hebei Medical University, Shijiazhuang 050011, China
3Department of Thoracic Surgery, Hebei General Hospital, Shijiazhuang 050057, China
4Graduate School,Hebei North University,Zhangjiakou 075000, China
* Correspondence:Jing Zhao, Department of Oncology, Hebei General Hospital, Shijiazhuang, Hebei, China. Email: zjzzmail@163.com
Abstract
Background: The morbidity and mortality of esophageal squamous cell carcinoma (ESCC) are among the top in the world and is characterized by insidious onset, late diagnosis, metastasis, treatment resistance and frequent recurrence. Therefore, the clinical prognosis of patients with ESCC is poor, with a 5-year survival rate of only 20%-30%. So, it is necessary to explore the indicators that can predict the prognosis of ESCC. Methods: The clinicopathological data of patients who were first diagnosed with ESCC at the Hebei General Hospital from July 2017 to December 2021 were retrospectively analyzed. Hematological indicators within 1 week of diagnosis were collected from patients, and platelet/high-density lipoprotein (Plt/HDL) were calculated based on. The cutoff value was obtained by receiver operating characteristic (ROC) curve. COX proportional-hazards model was performed for univariate and multifactorial analysis of prognostic factors affecting progression-free survival (PFS) and overall survival (OS) in ESCC, and Kaplan-Meier survival curve was used to evaluate the prognostic significance of Plt/HDL in ESCC patients. Results: A total of 274 patients were included, with a median PFS and OS of 21.32 months and 30.84 months, respectively. The median PFS of low and high groups were 25.59 months and 14.26 months, respectively. The median OS of the low and high groups was 31.27 months and 26.8 months, respectively. There were significant differences in FPS and OS between the two groups. Univariate and multivariate analyses showed that Plt/HDL had an independent prognostic effect on PFS and OS (P<0.05). Survival analysis showed a significant correlation between Plt/HDL and both PFS and OS (P<0.05). Lower Plt/HDL predicted longer PFS and OS. Conclusion: Plt/HDL is an independent prognostic factor for PFS and OS in patients with ESCC, and low Plt/HDL may predict longer PFS and OS. Therefore, Plt/HDL can predict the prognosis of patients with ESCC.
Keywords: ESCC, Plt/HDL, survival analysis, prognostic value
1.Introduction
ESCC is one of the deadliest malignancies. Because of its insidious onset, lack of typical symptoms and specific diagnostic methods, more than 90% of patients have progressed to the middle and late stages by the time of diagnosis, with poor quality of life.[1] The recurrence rate after radical radiotherapy, chemotherapy and surgery is more than 70%. The prognosis is poor, with a 5-year survival rate of only 20%-30%.[1] Therefore, how to effectively improve the prognosis of patients is an important issue in current clinical research, and it is of great value to adopt scientific and effective indicators to reasonably assess the survival and prognosis of ESCC patients.
The tumor microenvironment is influenced by several factors, among which relevant inflammatory, nutritional and immunological indicators play an important role. Several studies have found that hematological indicators are of great significance for the early diagnosis and prognosis of ESCC, and they have an important potential clinical value because they are easily evaluated, inexpensive and readily available prognostic biomarkers. In this study, we found that Plt/HDL is correlated with the prognosis of ESCC. Therefore, this paper will investigate the relationship between the Plt/HDL and the prognosis of ESCC, in order to provide a new direction for clinical treatment and diagnosis of ESCC patient prognosis. This research has been approved by the Ethics Committee of Hebei General Hospital(NO.2023117).
2. Information and methods
2.1 General data
The clinicopathological data of patients with ESCC first diagnosed in Hebei General Hospital from July 2017 to December 2021 were retrospectively analyzed. Inclusion criteria: (1) complete clinical data;(2) the pathological report was ESCC;(3) the results of hematological indicators were complete and obtained within 1 week before or after first diagnosis; (4) all data were obtained at first diagnosis and without receiving any antitumor-related treatment. Exclusion criteria: (1) missing hematological findings; (2) combined with serious cardiac, pulmonary, brain and other medical diseases; (3) combined with other malignant tumors or rheumatologic immune related diseases; (4) antitumor therapy was performed in other hospitals before he was admitted to our hospital. Finally, 274 ESCC patients were included, including 195 males and 79 females, aged 43-95 years.
2.2 Study methods
Baseline data and hematological indicators within 1 week of pathological diagnosis without treatment, and treatment status were retrospectively collected from 274 ESCC patients. Plt/HDL was calculated according to hematological indexes.
2.3 Follo-up
Follow-up was performed using outpatient review, telephone and case information inquiries. The primary endpoint was OS, which was defined as the time from the day of pathological diagnosis to death or the cut-off time for follow-up. The secondary endpoint was PFS, which was defined as the time from the day of pathological diagnosis to the time of disease progression or the cut-off time for follow-up. The interval between follow-up visits was 3 months. Two consecutive failed follow-up visits were considered deaths, and the date of death was the last follow-up time. Follow-up was at least 12 months, with a cut-off date of March 1, 2023.
2.4 Statistical methods
Statistical analysis was performed using R software. Using ROC curve analysis to obtain cutoff values. Using COX proportional-hazards model to perform univariate and multifactorial analysis of prognostic factors affecting ESCC. Using Kaplan-Meier and COX regression analysis were used to assess the prognostic significance of Plt/HDL. P < 0.05 was considered a statistically significant difference.
3. Results
3.1 Patient characteristics
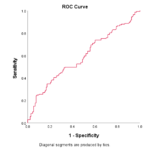
A total of 274 patients with ESCC were included, with an age range of 43-95 years. Male patients were 195 (71.2%) and 117 (42.7%) patients had a smoking history. According to clinical and pathological findings, 43 (15.7%) patients were high differentiation, and 33 (12.0%) and 94 (34.3%) patients had distant metastases and lymph-node metastases, respectively, at the time of diagnosis. In terms of treatment, 141 (51.5%) patients underwent surgery, 161 (58.8%) patients received pharmacological treatment, and 118 (43.1%) patients received radiotherapy. Population statistics and clinical information collected and baseline laboratory parameters are shown in Table 1. Optimal cutoff values based on ROC curves was 268.32 for Plt/HDL (Figure 1).
Table 1. Clinical Characteristics of Patients
| Characteristics | Level | Overall |
| N=274 | ||
| Gender (%) | Male | 195 (71.2) |
| Female | 79 (28.8) | |
| Age (%) | ≤60 | 49 (17.9) |
| >60 | 225 (82.1) | |
| BMI (%) | ≤24 | 166 (60.6) |
| >24 | 108 (39.4) | |
| Smoking (%) | NO | 157 (57.3) |
| YES | 117 (42.7) | |
| Drinking (%) | NO | 177 (64.6) |
| YES | 97 (35.4) | |
| Differentiation (%) | Low-medium | 231(84.3) |
| High | 43 (15.7) | |
| Metastasis (%) | NO | 241(88.0) |
| YES | 33 (12.0) | |
| Lymph-node metastasis (%) | NO | 180 (65.7) |
| YES | 94 (34.3) | |
| Surgery (%) | NO | 133 (48.5) |
| YES | 141 (51.5) | |
| Drug (%) | NO | 113 (41.2) |
| YES | 161 (58.8) | |
| Radiotherapy (%) | NO | 156 (56.9) |
| YES | 118 (43.1) | |
| Plt/HDL (%) | ≤268.32 | 202 (73.7) |
| >268.32 | 72 (26.3) |
Figure 1. ROC curves of Plt/HDL cutoff values were determined.
3.2 Relationship between Plt/HDL and clinicopathological characteristics of ESCC patients
We analyzed the relationship between Plt/HDL and clinicopathological characteristics of ESCC patients and the results are shown in Table 2. Differentiation (P=0.011), Metastasis (P=0.001), LNM (P=0.047), Surgery (P<0.001), Radiotherapy (P=0.038) were statistically different from the low and high PPS groups.
Table 2. Relationship Between Patient Characteristics and Plt/HDL
| Characteristics | Level | Overall | Low Plt/HDL | High Plt/HDL | P |
| N=274 | N=202 | N=72 | |||
| Gender (%) | Male | 195 (71.2) | 135 (66.8) | 60 (83.3) | 0.012 |
| Female | 79 (28.8) | 67 (33.2) | 12 (16.7) | ||
| Age (%) | ≤60 | 49 (17.9) | 32 (15.8) | 17 (23.6) | 0.194 |
| >60 | 225 (82.1) | 170 (84.2) | 55 (76.4) | ||
| BMI (%) | ≤24 | 166 (60.6) | 125 (61.9) | 41 (56.9) | 0.551 |
| >24 | 108 (39.4) | 77 (38.1) | 31 (43.1) | ||
| Smoking (%) | NO | 157 (57.3) | 127 (62.9) | 30 (41.7) | 0.003 |
| YES | 117 (42.7) | 75 (37.1) | 42 (58.3) | ||
| Drinking (%) | NO | 177 (64.6) | 135 (66.8) | 42 (58.3) | 0.250 |
| YES | 97 (35.4) | 67 (33.2) | 30 (41.7) | ||
| Differentiation (%) | Low-medium | 231 (84.3) | 169 (83.7) | 62 (86.1) | 0.763 |
| High | 43 (15.7) | 33 (16.3) | 10 (13.9) | ||
| Metastasis (%) | NO | 241 (88.0) | 184 (91.1) | 57 (79.2) | 0.014 |
| YES | 33 (12.0) | 18 (8.9) | 15 (20.8) | ||
| Lymph-node metastasis (%) | NO | 180 (65.7) | 136 (67.3) | 44 (61.1) | 0.418 |
| YES | 94 (34.3) | 66 (32.7) | 28 (38.9) | ||
| Surgery (%) | NO | 133 (48.5) | 89 (44.1) | 44 (61.1) | 0.019 |
| YES | 141 (51.5) | 113 (55.9) | 28 (38.9) | ||
| Drug (%) | NO | 113 (41.2) | 88 (43.6) | 25 (34.7) | 0.242 |
| YES | 161 (58.8) | 114 (56.4) | 47 (65.3) | ||
| Radiotherapy (%) | NO | 156 (56.9) | 118 (58.4) | 38 (52.8) | 0.490 |
| YES | 118 (43.1) | 84 (41.6) | 34 (47.2) |
3.3 Univariate and multivariate analysis of PFS in ESCC patients
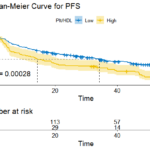
The median PFS for the 274 participants was 21.32 months. The median PFS of low and high groups were 25.59 months and 14.26 months. Patients in the low Plt/HDL had significantly longer PFS than those in the high group. According to the results of univariate and multifactorial analysis, high differentiation, metastasis, lymph-node metastasis, radiotherapy, and low Plt/HDL predicted longer FPS in ESCC patients. Surgery was significant only in the univariate analysis. These results suggest that the above factors may be independent prognostic factors in ESCC patients (all P<0.05) (Table 3). The survival curves of PFS drawn by Kaplan-Meier survival analysis are shown in Figure 2, indicating that patients in the low Plt/HDL had longer PFS (P<0.001).
Table 3. Univariate and Multivariate Analysis for PFS
| Characteristics | Univariable Analysis | Multivariable Analysis | ||
| P | HR (95%CI) | P | HR (95%CI) | |
| Gender | 0.933 | 1.01 (0.74-1.4) | NA | NA |
| Age | 0.347 | 1.21 (0.81-1.81) | NA | NA |
| BMI | 0.269 | 0.84 (0.62-1.14) | NA | NA |
| Smoking | 0.211 | 1.21 (0.9-1.62) | NA | NA |
| Drinking | 0.998 | 1 (0.74-1.36) | NA | NA |
| Differentiation | 0 | 0.33 (0.2-0.54) | 0.0008 | 0.42 (0.26-0.7) |
| Metastasis | 0 | 3.72 (2.52-5.51) | 0.0017 | 2.11 (1.32-3.37) |
| LNM | 0 | 2.21 (1.63-3) | 0.0005 | 1.79 (1.29-2.49) |
| Surgery | 0 | 0.54 (0.4-0.72) | 0.1964 | 0.79 (0.56-1.13) |
| Drug | 0.102 | 1.29 (0.95-1.74) | NA | NA |
| Radiotherapy | 0 | 1.99 (1.48-2.68) | 0.0028 | 1.66 (1.19-2.32) |
| Plt/HDL | 0 | 1.77 (1.3-2.42) | 0.0477 | 1.39 (1-1.94) |
Figure 2. Kaplan-Maier curves of PFS for Plt/HDL
3.4 Univariate and multivariate analysis of OS in ESCC patients
The median OS for the 274 participants was 30.84 months. The median OS of low and high groups were 31.27 months and 26.8 months, respectively. Patients in the low Plt/HDL had significantly longer OS than those in the high group. According to the results of univariate and multifactorial analyses, high differentiation, metastasis, lymph-node metastasis, surgery, and low Plt/HDL predicted longer OS in ESCC patients. These results suggest that the above factors may be independent prognostic factors in ESCC patients (all P<0.05) (Table 4). The survival curves of OS drawn by Kaplan-Meier survival analysis are shown in Figure 3, indicating that patients in the low Plt/HDL had longer OS (P=0.001).
Table 4. Univariate and Multivariate Analysis for OS
| Characteristics | Univariable Analysis | Multivariable Analysis | ||
| P | HR (95%CI) | P | HR (95%CI) | |
| Gender | 0.407 | 1.16 (0.82-1.65) | NA | NA |
| Age | 0.095 | 1.49 (0.93-2.37) | NA | NA |
| BMI | 0.602 | 0.91 (0.65-1.28) | NA | NA |
| Smoking | 0.781 | 1.05 (0.75-1.46) | NA | NA |
| Drinking | 0.119 | 0.75 (0.53-1.08) | NA | NA |
| Differentiation | 0 | 0.26 (0.14-0.48) | 0.0001 | 0.29 (0.16-0.52) |
| Metastasis | 0 | 3.58 (2.33-5.5) | 0.0405 | 1.69 (1.02-2.8) |
| LNM | 0.002 | 1.72 (1.23-2.42) | 0.0383 | 1.47 (1.02-2.11) |
| Surgery | 0 | 0.43 (0.3-0.6) | 0.0007 | 0.5 (0.33-0.75) |
| Drug | 0.862 | 1.03 (0.74-1.44) | NA | NA |
| Radiotherapy | 0.007 | 1.58 (1.13-2.2) | 0.8789 | 1.03 (0.71-1.49) |
| Plt/HDL | 0.001 | 1.78 (1.25-2.52) | 0.0439 | 1.46 (1.01-2.11) |
Figure 3. Kaplan-Maier curves of OS for Plt/HDL
4. Discussion
The prognostic value of inflammatory and nutritional parameters has been de monstrated in many studies. Although these parameters are important prognostic factors in tumor patients, the analysis of individual parameters often cannot provide sufficient predictive power in clinical practice. So it is necessary to combine multiple parameters to improve the accuracy of prognosis prediction. Through a large number of data analysis, we found that Plt/HDL had a certain predictive value for the prognosis of patients with ESCC. In this study, we integrated multiple biomarkers to predict the relationship between peripheral blood biomarkers and clinical outcomes in ESCC patients. Our data showed that high Plt/HDL was associated with gender, smoking, metastases, no surgery was performed, and poorer survival status.
In the tumor microenvironment, multiple immune cell regulators and systemic inflammatory markers are associated with tumor development. Platelets are involved in the genesis and development of tumors. Platelets induce tumor growth and invasion by secreting a variety of growth factors and small molecules, driving epithelial interstitium transformation (EMT) processes, secreting pro-angiogenic factors such as VEGF to induce angiogenesis, and inducing Cyclooxygenase-2 (COX-2), which has oncogenic effect. [2, 3]Platelets not only promote the development of tumor, but also induce immune escape of tumor cells. Platelets induce immune escape of tumor cells by inhibiting NK cell activation and function and T cell proliferation, and protect circulating tumor cells (CTCs) against NK cell and TNFα induced cell death. [3, 4]It can be speculated that the immunosuppressive effect of platelets may weaken the efficacy of immunotherapy to some extent, which raises higher requirements and challenges for screening patients receiving immunotherapy, strengthening the management of platelet transfusion products, and applying multi-pathway antitumor therapy strategies. However, the extent of platelet immunosuppressive effect in tumor microenvironment and the range in which platelet can exert the maximum immunosuppressive effect still need to be further explored. HDL is a multifunctional lipoprotein, which has anti-oxidant, anti-apoptosis, regulation of cytokine synthesis, and stimulation of cell differentiation and migration, and decreased levels play an important role in the occurrence and development of tumors.[5, 6] Related studies have shown that HDL is a clinical prognostic factor for lung cancer and breast cancer.
We explored the value of the Plt/HDL, which reflects the immunoinflammatory and nutritional status of patients and predicts the prognosis of ESCC patients. We found that Plt/HDL was significantly correlated with the prognosis of ESCC patients through univariate and multivariate analysis of PFS and OS in ESCC patients. Also, the survival curves showed that patients with low Plt/HDL group had longer survival. We conclude that Plt/HDL is an independent prognostic factor for ESCC patients.
5. Innovations and shortcomings
We are the first article to study the prognostic value of Plt/HDL in ESCC. Relative indicators of Plt/HDL are extremely easy to obtain in clinically,which can better predict the prognosis of patients. However, there are some limitations of this study that need to be mentioned. First, the patient sample size needs to be increased and patients with different cancer types need to be selected to reduce the potential bias in the retrospective study design. Second, the choice of treatment modality can affect OS and thus the predictive accuracy of Plt/HDL. Therefore, the results of this study need to be validated by a larger sample size, analysis and more fully clinicopathological and survival data of prospective studies.
6. Summary
Plt/HDL, as a simple, practical and easily available prediction indicator, is an independent prognostic factor for the survival in ESCC patients. Lower Plt/HDL predicts longer survival, We are currently studying this tool in ESCC patients to improve the prognostic status of patients with a high Plt/HDL.
Author Contributions
Shumin Cao: Collected and analyzed data, wrote articles; Shuangqing Chen: Analyzed data; Shuang Zhang: Collected data; Qingxin Zhao: Sort out data; Jing Zhao: Revised the article.
Ethical approval
Approved by the Ethics Committee of Hebei General Hospital (NO.2023117).
Participation Consent
All authors of this article participated and agreed to publish.
Acknowledgments
Thanks to all the teachers and colleagues for their help. Thanks for the support from Hebei Medical Science Research Project in 2022 (20220071).
Conflict of interest
There is no conflict of interest in this article.
References
- ZHENG B, LI J, ZHANG M, et al. Analysis of immunotherapeutic response-related signatures in esophageal squamous-cell carcinoma[J]. Front Immunol, 2023,14: 1117658.
- SCHLESINGER M. Role of platelets and platelet receptors in cancer metastasis[J]. J Hematol Oncol, 2018,11(1): 125.
- HAEMMERLE M, STONE R L, MENTER D G, et al. The Platelet Lifeline to Cancer: Challenges and Opportunities[J]. Cancer Cell, 2018,33(6): 965-983.
- YU L, GUO Y, CHANG Z, et al. Bidirectional Interaction Between Cancer Cells and Platelets Provides Potential Strategies for Cancer Therapies[J]. Front Oncol, 2021,11: 764119.
- MAZZUFERI G, BACCHETTI T, ISLAM M O, et al. High density lipoproteins and oxidative stress in breast cancer[J]. Lipids Health Dis, 2021,20(1): 143.
- MA J, BAI Y, LIU M, et al. Pretreatment HDL-C and ApoA1 are predictive biomarkers of progression-free survival in patients with EGFR mutated advanced non-small cell lung cancer treated with TKI[J]. Thorac Cancer, 2022,13(8): 1126-1135.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/