J Med Discov (2020); 5(4):jmd20079; DOI:10.24262/jmd.5.4.20079; Received December 03rd, 2020, Revised December 08th, 2020, Accepted December 15th, 2020 , Published December 18th, 2020.
Oncolytic adenovirus armed with OVA and OVA peptides vaccines can effectively treat spinal metastases in murine model Novel therapy strategy for spinal metastases
Xiaorui Zhang1, Xinyu Feng1, *
1 Shanghai Institute of Biochemistry and Cell Biology, CAS, 320 Yueyang Road, Shanghai, 200023, China.
* Correspondence:Xinyu Feng,Shanghai Institute of Biochemistry and Cell Biology, CAS, 320 Yueyang Road, Shanghai, 200023, China.E-mail: aoun_fengxinyu@hotmail.com
Abstract
Spinal metastases are the most common type of bone metastases, occurring in 30%–70% of cancer patients. Oncolytic viruses represent a novel strategy for cancer therapy; however, the effects of clinical application of adenoviruses remain limited. We therefore examined the potency of a new oncolytic adenovirus (oAds) armed with the ovalbumin (OVA) gene, combined with OVA-specific peptide vaccines, in a spinal metastasis mouse model. oAds and oAds-OVA were constructed and compared in A549 and MC38 cells. Insertion of the OVA expression cassette did not reduce the potency of the virus in vitro. We then tested the function of oAds-OVA in an A549 mouse xenograft model. Intratumoral injection of oAds-OVA increased lymphocyte infiltration and specifically expressed OVA at the injection site. We also examined the anti-tumor effect of OAds-OVA combined with OVA peptides in a spinal metastasis model. The combination of oAds-OVA and OVA peptides prolonged survival compared with oAds-OVA. In summary, the combination of oAds-OVA and OVA peptides had an anti-tumor effect in a spinal metastasis model, through increasing the tumor-specific immune response. The combination was shown to be safe in a mouse model. The oAds-OVA and OVA peptides combination has potential clinical applications for the treatment of spinal metastases.
Keywords:Oncolytic adenovirus, ovalbumin-specific vaccine, tumor-specific antigen, spinal metastasis
Introduction
Spinal metastases are the most common type of bone metastases, occurring in nearly 30%–50% of cancer patients [1]. During cancer development, primary tumor cells migrate and establish secondary tumors in the vertebral column, with negative effects on the patient’s daily life. Although the survival rates of the primary tumors differ, the 5-year survival rate of patients with spinal metastases is about 50% [2, 3]. Traditional therapies to prevent tumor recurrence are difficult, and have the potential for neurological damage [4-6].
Various immunotherapies have recently shown great potency in the treatment of advanced cancers [7]. Neoantigen therapy is a novel immunotherapy based on predicted tumor-specific antigens, and uses synthesized tumor-specific antigens to overcome the cancer immune escape by triggering the immune system [8, 9]. However, neoantigen prediction and synthesis are time-consuming, and many cancer patients cannot wait. We therefore aimed to create a vehicle to cause tumor cells to present tumor-specific antigens, which can then act as a target for peptide vaccines.
Oncolytic viruses represent another kind of immunotherapy in which the modified virus can only replicate in cancer cells [10, 11]. The host cells undergo lysis during virus replication and are then eradicated by the immune system, which is activated by the virus. Adenoviruses have a long history of modification as oncolytic viruses. Deleting the E1B 55K protein confines replication of the oncolytic adenovirus (oAds) to p53 mutant cells [12, 13]. Oncolytic viruses are also ideal tumor-specific vectors for the delivery of exogenous genes. We tested the anti-tumor effect and safety of oAds armed with ovalbumin (OVA), as a well-validated antigen, both in vitro and in vivo.
Materials and methods
Animals and ethics statement
Thirty female BALB/c nude mice (6–8 weeks old) and 80 female C57BL/6 mice (6–8 weeks old) were maintained in a light- and temperature-controlled room. All experimental procedures were approved by the Institutional Animal Care and Use Committee of the Chinese Academy of Science (No. HRJ-FFS-ON-20200127-01) under specific pathogen-free conditions.
Cell lines and culture conditions
The cancer cell lines A549 and MC38 were purchased from iCell Bioscience (China). A549 cells were maintained in Ham’s F12-K medium (21127030, Gibco, USA) and MC38 cells were maintained in RPMI-1640 medium (61870036, Gibco). Both media were supplemented with 10% fetal bovine serum (FBS; 16000-044; Gibco), 10,000 U/mL penicillin, and 10 mg/mL streptomycin (V900929, Sigma-Aldrich, USA). The cells were incubated in a humidified atmosphere containing 5% CO2 at 37°C.
oAds preparation
Basic AdMax system plasmids containing a copy of the Ad5 genome identical to the Adenovirus Type 5 Reference Material (GenBank AY339865) were purchased from Genechem (China). E1B 55K was deleted to construct the oAds, and oAds-OVA was constructed by replacing E1B 55K by hTERT-OVA-SV40. The vectors were transfected into HEK-293 cells and harvested after more than half the cells were dead. Virus titers were determined by median tissue culture infective dose assay.
Cell viability assay
A549 (800 cells per well) and MC38 (800 cells per well) cells were added in 96-well plates and allowed to grow overnight. A549 cells were infected with three oAds at multiplicities of infection (MOIs) of 1, 2, 4, 8, 16, 32, 64, 128, and 256. MC38 cells were infected with oAds or oAds-OVA at MOIs of 7, 17, 45, 110, 270, 650, 1500, and 5000. All virus samples were diluted into 100 μL medium before use and 100 μL medium was added to negative controls. Each MOI was repeated three times. The viruses and cells were co-cultured for 96 h, and 10 μL CCK-8 (CK04; Dojindo, Japan) was then added to each well to measure cell viability. The plates were incubated for 4 h and the absorbance was measured at 450 nm using a microplate reader to evaluate the 50% inhibitive concentration (IC50) for each assay.
Xenograft models
Thirty female BALB/c nude mice (6–8 weeks old) were selected to construct an A549 xenograft model. The xenograft model was established by subcutaneous (SC) injection of A549 cells (5106/100 μL) into the right leg, after checking the cell viability by Trypan blue staining (15250061; Invitrogen, USA). When the tumors reached nearly 100 mm3, the mice were divided into three groups (n=5 each) using Study Director (Studylog System, Inc., USA) and the spare mice were sacrificed. Mice in the oAds and oAds-OVA groups received intratumoral injection of 50 μL oAds (11010 plaque-forming unit (pfu)/mL) and oAds-OVA on days 1, 3, and 5, respectively. Mice in the control group received intratumoral injection of 50 μL phosphate-buffered saline (PBS) on days 1, 3, and 5. The tumor volume was calculated as (length × width2)/2 and measured every 3 days. All mice were sacrificed after 28 days or when the tumor reached 2000 mm3.
Spinal metastasis model
Eighty female C57BL/6 mice (6–8 weeks old) were selected to create an MC-38 spinal metastases model. Spinal metastases were established by subcutaneous injection of MC-38 cells (1105/100 μL) into the right ventricular lumen of the heart. Mice were anesthetized with 2% isoflurane. At 6 days after injection, the mice were divided into three groups (n=8 each) using Study Director (Studylog System, Inc.) and the remaining mice were sacrificed. Mice in the oAds and oAds-OVA groups received intravenous injection via the tail vein of 100 μL oAds (11011 pfu/mL) and 100 μL oAds-OVA (11011 pfu/mL) on days1, 3, and 5 after injection, respectively. Mice in the control group were injected with 100 μL PBS in the same way. OVA peptide (SIINFEKL) was synthesized by GL Biochem (China). All mice were injected with OVA peptides 2 weeks before grouping. OVA peptides 30 μg and 50 μg Poly(I:C) (B5551, APEXBio, USA) were injected SC at the inner side of each thigh every 3 days for five doses. All surviving mice were sacrificed 21 days after injection.
Cytotoxic T lymphocyte (CTL) killing effect assay
CTLs were extracted from the spleens of spinal metastasis model mice at day 21 and maintained in RPMI-1640 with 10% FBS, interleukin-7 (C086; Novoprotein, China) 10 ng/mL, interleukin-2 (CK24; Novoprotein) 10 ng/mL, and OVA peptides (5 ng/mL). The cells were incubated in a humidified atmosphere containing 5% CO2 at 37°C for 2–3 weeks. MC38 cells (500 cells per well) were seeded into plates and allowed to grow overnight, followed by the addition of 10 MOI oAds-OVA into each well. CTLs from each group were added into each well at CTL target ratios of 1:1, 1:2, 1:4, 1:8, 1:16, 1:32, 1:64, and 1:128. The percentage of CTLs was tested by ELISpot assay (3321-2A; Mabtech, USA). Splenocytes from each group were mixed and added into each well (2105 cells/well). Each group was repeated three times. ELISpot assays were tested as per standard protocol. The specific immune response in each group was compared by spot-formation count (SFC).
Immunohistochemistry (IHC)
Tumors were extracted from A549 model mice at 28 days, fixed in 10% neutral buffered formalin for 24 h, embedded in paraffin, and sliced at 3 μm thickness. The sections were deparaffinized, rehydrated, dewaxed, and graded debenzolization. The sections were then heated to induce the antigens and cooled for 30 min. CD45 (1:1000, ab185744; Abcam, USA) and OVA (1:1000, ab181688; Abcam) antibodies were used as per protocol.
Statistical analysis
The results were analyzed by analysis of variance and Student’s t-test. All data were presented as mean ± standard error of mean. IC50 was calculated by four-parameter logistic regression. Survival curves were compared by the log-rank test. All analyses were conducted using GraphPad Prism 7.0 software (GraphPad software, USA).
Results
OVA-armed oAds did not reduce anti-tumor effect of oAds in vitro
The effects of the harvested virus were tested in A549 and MC38 cells to determine if the OVA expression cassette reduced the potency of the oAds. The IC50 (MOI) values of oAds and oAds-OVA in A549 cells were 25.72 and 20.02, respectively (Fig. 1A), and the equivalent values in MC38 cells were 16.59 and 50.35, respectively (Fig. 1B). There were no significant differences in the potencies of oAds and oAds-OVA, indicating that the OVA expression cassette did not reduce the potency of oAds. The anti-tumor effects of oAds were similar in the human cancer cell line A549 and the mouse cancer cell line MC38, suggesting that they could be used in a syngeneic model.
Figure 1. The potency of MMAD-IL-13. A. oAds and oAds-OVA showed similar IC50 values in A549 cells. B. oAds and oAds-OVA showed similar IC50 values in MC38 cells.
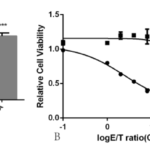
oAds-OVA and OVA peptides combination effectively killed tumor cells in vitro
We investigated the synergistic effect between oAds-OVA and OVA peptides. OVA-specific T cells in splenocytes harvested from each group in the spinal metastases model were compared by ELISpot (Fig. 2A). The SFC was higher in the oAds-OVA group compared with the oAds and control groups (P<0.01), with no significant difference in SFCs between the control and oAds groups (P>0.05). We also compared the CTL killing effect in an in vitro model with co-cultured splenocytes from each group of mice in the MC38 spinal metastasis model. CTLs from the oAds-OVA plus OVA peptides group showed obvious killing effects (Fig. 2B), while the effects of CTLs from the oAds-OVA and control groups were similar. These results demonstrated a synergistic effect of oAds-OVA and OVA peptides in the MC-38 spinal metastasis model.
Figure 2. CTL killing assay. The percentages of OVA-specific T cells were determined in splenocytes from MC-38 spinal metastasis mice at day 21. A. Percentages of specific T cells compared by ELISpot assay showed significantly higher SFC in the oAds-OVA group compared with the oAds and control groups. B. MC38 mice were infected with oAds-OVA or oAds at 10 MOI before adding CTLs. The IC50 was significantly higher in the oAds-OVA group compared with the oAds and control groups.
oAds inhibited A549 proliferation in vivo
We confirmed the function of oAds-OVA by intratumoral injection of oAds-OVA and oAds in an A549 mouse xenograft model. Tumor size increased in the control group than 2000 mm3 at 28 days (Fig. 3A), compared with 792.3±64.76 and 862.1±113.0 mm3 in the oAds and oAds-OVA groups, respectively. Tumor volumes were significantly smaller in the oAds and oAds-OVA groups compared with the control group (P<0.01). The body weights of mice in the control, oAds, and oAds-OVA groups were 24.66±0.46, 23.88±0.86, and 24.20±0.46 mg, respectively (Fig. 3B). oAds and oAds-OVA thus had similar significant tumor-growth-inhibition effects (P>0.05) without affecting body weight (P>0.05).
Figure 3. In vivo study in A549 model mice. Samples were collected from each group at day 28 for IHC examination. Sections were photographed under a 20× objective lens. A. Tumor-growth inhibition was tested by the terminal. Tumors were significantly smaller in the oAds and oAds-OVA groups compared with the control group (P<0.01). B. Virus safety was examined in vivo by comparing the body weights of A549 xenograft model mice. There was no significant difference in body weight among the groups (P>0.05). C. CD45-stained control group; D. OVA-stained control group; E. CD45-stained oAds group; F. OVA-stained oAds group; G. CD45-stained oAds-OVA group; H. OVA-stained oAds-OVA group.
oAds-OVA expressed OVA at the injection site and increased leukocyte infiltration
We examined OVA expression and leukocyte infiltration by IHC. Few infiltrating leukocytes were detected in the control group, determined by CD45 staining (Fig. 3C). The oncolytic virus lysed the tumor cells at the injection site and expressed OVA during virus replication (Fig. 3H), while no OVA expression was detected in the oAds and control groups (Fig. 3D, F). oAds-OVA and oAds also increased leukocyte infiltration in the whole tumor (Fig. 3E, G).
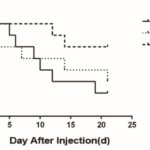
oAds-OVA plus OVA peptides prolonged survival of spinal metastasis model mice
We examined the effect of the combination of oAds-OVA plus OVA peptides in spinal metastasis model mice. Mice in the oAds-OVA group had a significantly better survival rate than mice in the oAds and control groups (P<0.05), while the survival rates in the oAds-OVA and control groups were similar (P>0.05). The mean survival periods of mice in the oAds-OVA, oAds, and control groups were 21, 17.5, and 11 days, respectively. Six of eight mice in the oAds-OVA group had died by the end of the experiment (survival rate: 25%), compared with two of eight in the oAds group (survival rate: 75%) and three of eight in the control group (survival rate: 37.5%) (Fig. 4).
Figure 4. Survival of MC38 spinal metastasis model mice. The survival rate of mice in the oAds-OVA group was significantly higher than in the control group (P<0.05). There was no significnt difference in survival rates between the oAds and control groups (P>0.05).
Discussion
Recent improvements in early detection and the emergence of novel treatments have increased the life expectancy of patients with spinal metastases. However, treatment of spinal metastases needs to take account of several factors, including the type of primary tumor and the general condition of the patient [3]. A previous meta-analysis [1, 14, 15] indicated that the survival rates of patients with spinal metastases were affected by the type of primary tumor. However, more effective and widely available treatments are urgently needed.
Since the first application of oncolytic viruses in 1995, improving their efficacy has been a focus of research. Cancer-targeting gene-viro-therapy [16-19] is one of the most promising strategies for clinical application. Modified oncolytic viruses armed with a gene to increase their efficacy can selectively kill tumor cells and express cytokines or antibodies [20]. Adenoviruses are the most widely used virus vectors, with relatively rapid clearance in vivo [21], which improves safety but also reduces their efficacy [10]. We therefore used adenovirus to express OVA to label tumor cells in vivo. OVA is a commonly used research model in cancer vaccines [22], which can also induce autoimmune diseases such as asthma [23, 24]. The hTERT promotor was used to restrict expression to the tumor [25, 26], and IHC confirmed that OVA was only expressed at the injection site. However, A549 nude mice lack mature T cells, and OVA expression did thus not exert its full effect in an A549 model.
Oncolytic viruses can also kill tumor cells by altering the tumor microenvironment [27, 28], which includes vascular proliferation and immune inhibitors [29]. Oncolytic viruses are exogenous substances that can trigger the host immune response to improve immune infiltration of the tumor. Virus replication can also lyse the host cells and release specific tumor antigens, thus circumventing tumor immune escape. IHC detection of CD45 confirmed that the oncolytic virus improved immune infiltration of the whole tumor.
The synergistic effect of oAds-OVA and OVA peptides was tested in an MC38 mouse spinal metastasis model. The oncolytic virus recruited and activated tumor-specific T cells. This help the specific T cells induced by OVA peptide vaccine given before recognized the tumor cells labeled by oAds-OVA. The tumor cells were then recognized by CD8+ T cells, which induced apoptosis [30]. Replication of oAds expressing adenovirus death protein can exacerbate host-cell death [31], and in the absence of E1B 55K, oAds are unable to block apoptosis via the classical tp53-induced pathway [13]. The lysed tumor cells also release tumor-specific antigens that are recognized by the immune system. This cycle of effects supports the rapid anti-tumor action at the metastasis site.
The MC38 spinal metastasis model confirmed the efficacy of the above mechanism in vivo; however further studies are needed to confirm its clinical effect. Further studies are also needed to address the high seroprevalence of Ad5 and the potential safety problems of OVA.
Conclusion
In summary, we created a new oAds armed with the OVA gene and showed that the combination of this oAds-OVA with OVA peptides had beneficial effects in a mouse model of spinal metastasis, through increasing the tumor-specific immune response. The combination was also safe in this mouse model. This oAds-OVA plus OVA peptides combination thus has potential clinical applications for the treatment of spinal metastases.
Conflict of interest
None
Acknowledgments
None
References
- Galgano, J. Fridley, A. Oyelese, A. Telfian, T. Kosztowski, D. Choi, et al. Surgical management of spinal metastases. Expert Rev Anticancer Ther. 2018; 18 (5): 463-472.
- M. Trilling, H. Cho, M.A. Ugas, S. Saeed, A. Katunda, W. Jerjes, et al. Spinal metastasis in head and neck cancer. Head Neck Oncol. 2012; 4 36.
- M. Kwon, K.S. Kim, S.U. Kuh, D.K. Chin, B.H. Jin, Y.E. Cho. Survival rate and neurological outcome after operation for advanced spinal metastasis (Tomita’s classification > or = type 4). Yonsei Med J. 2009; 50 (5): 689-696.
- A. Kumar, K.K. Peck, S. Karimi, E. Lis, A.I. Holodny, M.H. Bilsky, et al. A Pilot Study Evaluating the Use of Dynamic Contrast-Enhanced Perfusion MRI to Predict Local Recurrence After Radiosurgery on Spinal Metastases. Technol Cancer Res Treat. 2017; 1533034617705715.
- Abdelbaky, H. Eltahawy. Neurological Outcome Following Surgical Treatment of Spinal Metastases. Asian J Neurosurg. 2018; 13 (2): 247-249.
- J. Andrade, SCM. Martins, C. Formentin, O. Turolo, V.L. Vasconcelos, E. Ghizoni, et al. Neurological Outcome and Complications in Patients with Surgically Treated Spinal Metastases. Spine (Phila Pa 1976). 2019;
- J. Bergman. Cancer Immunotherapies. Vet Clin North Am Small Anim Pract. 2019; 49 (5): 881-902.
- Li, S.P. Goedegebuure, W.E. Gillanders. Preclinical and clinical development of neoantigen vaccines. Ann Oncol. 2017; 28 (suppl_12): xii11-xii17.
- Guo, K. Lei, L. Tang. Neoantigen Vaccine Delivery for Personalized Anticancer Immunotherapy. Front Immunol. 2018; 9 1499.
- T. Martin, J.C. Bell. Oncolytic Virus Combination Therapy: Killing One Bird with Two Stones. Mol Ther. 2018; 26 (6): 1414-1422.
- Raja, J.M. Ludwig, S.N. Gettinger, K.A. Schalper, H.S. Kim. Oncolytic virus immunotherapy: future prospects for oncology. J Immunother Cancer. 2018; 6 (1): 140.
- Cherubini, T. Petouchoff, M. Grossi, S. Piersanti, E. Cundari, I. Saggio. E1B55K-deleted adenovirus (ONYX-015) overrides G1/S and G2/M checkpoints and causes mitotic catastrophe and endoreduplication in p53-proficient normal cells. Cell Cycle. 2006; 5 (19): 2244-2252.
- A. Thomas, T. Nyanhete, I. Tuero, D. Venzon, M. Robert-Guroff. Beyond Oncolytics: E1B55K-Deleted Adenovirus as a Vaccine Delivery Vector. PLoS One. 2016; 11 (7): e0158505.
- Gong, L. Xu, H. Zhuang, L. Jiang, F. Wei, Z. Liu, et al. Efficacy and safety of different fractions in stereotactic body radiotherapy for spinal metastases: A systematic review. Cancer Med. 2019; 8 (14): 6176-6184.
- Sutcliffe, M. Connock, D. Shyangdan, R. Court, N.B. Kandala, A. Clarke. A systematic review of evidence on malignant spinal metastases: natural history and technologies for identifying patients at high risk of vertebral fracture and spinal cord compression. Health Technol Assess. 2013; 17 (42): 1-274.
- Cao, R. Wei, X. Liu, Y. Zeng, H. Huang, M. Ding, et al. Cancer targeting gene-viro-therapy specific for liver cancer by alpha-fetoprotein-controlled oncolytic adenovirus expression of SOCS3 and IL-24. Acta Biochim Biophys Sin (Shanghai). 2011; 43 (10): 813-821.
- Cao, M. Yang, R.C. Wei, Y. Zeng, J.F. Gu, W.D. Huang, et al. Cancer targeting Gene-Viro-Therapy of liver carcinoma by dual-regulated oncolytic adenovirus armed with TRAIL gene. Gene Ther. 2011; 18 (8): 765-777.
- Liu, X. Cao, R. Wei, Y. Cai, H. Li, J. Gui, et al. Gene-viro-therapy targeting liver cancer by a dual-regulated oncolytic adenoviral vector harboring IL-24 and TRAIL. Cancer Gene Ther. 2012; 19 (1): 49-57.
- Y. Liu, H.G. Li, K.J. Zhang, J.F. Gu. Strategy of Cancer Targeting Gene-Viro-Therapy (CTGVT) a trend in both cancer gene therapy and cancer virotherapy. Curr Pharm Biotechnol. 2012; 13 (9): 1761-1767.
- M. Pearl, J.M. Markert, K.A. Cassady, M.G. Ghonime. Oncolytic Virus-Based Cytokine Expression to Improve Immune Activity in Brain and Solid Tumors. Mol Ther Oncolytics. 2019; 13 14-21.
- Varghese, Y. Mikyas, P.L. Stewart, R. Ralston. Postentry neutralization of adenovirus type 5 by an antihexon antibody. J Virol. 2004; 78 (22): 12320-12332.
- Zhu, F. Ge, L. Yang, W. Li, S. Wei, Y. Tao, et al. Alginate Particles with Ovalbumin (OVA) Peptide Can Serve as a Carrier and Adjuvant for Immune Therapy in B16-OVA Cancer Model. Med Sci Monit Basic Res. 2017; 23 166-172.
- Q. Luo, J.W. Zhong, S.Y. Qiu, M. Zhi, L.Q. Yang, Y.L. Zhou, et al. A20-OVA Nanoparticles Inhibit Allergic Asthma in a Murine Model. Inflammation. 2020;
- Maruthamuthu, L.J.K. Henry, M.K. Ramar, R. Kandasamy. Myxopyrum serratulum ameliorates airway inflammation in LPS-stimulated RAW 264.7 macrophages and OVA-induced murine model of allergic asthma. J Ethnopharmacol. 2020; 255 112369.
- Fang. Targeting apoptosis to cancer via hTERT promoter. Cancer Biol Ther. 2006; 5 (11): 1554-1555.
- Li, G. Pan, Y. Chen, Q. Yang, T. Hao, L. Zhao, et al. Inhibitor of the human telomerase reverse trancriptase (hTERT) gene promoter induces cell apoptosis via a mitochondrial-dependent pathway. Eur J Med Chem. 2018; 145 370-378.
- Altomonte, O. Ebert. Sorting Out Pandora’s Box: Discerning the Dynamic Roles of Liver Microenvironment in Oncolytic Virus Therapy for Hepatocellular Carcinoma. Front Oncol. 2014; 4 85.
- Kuhn, P. Harden, M. Bauzon, C. Chartier, J. Nye, S. Thorne, et al. Directed evolution generates a novel oncolytic virus for the treatment of colon cancer. PLoS One. 2008; 3 (6): e2409.
- Arneth. Tumor Microenvironment. Medicina (Kaunas). 2019; 56 (1):
- D. Shore, M.P. Morrow, T. McMullan, K.A. Kraynyak, A. Sylvester, K. Bhatt, et al. CD8(+) T Cells Impact Rising PSA in Biochemically Relapsed Cancer Patients Using Immunotherapy Targeting Tumor-Associated Antigens. Mol Ther. 2020;
- K. Murali, D.A. Ornelles, L.R. Gooding, H.T. Wilms, W. Huang, A.E. Tollefson, et al. Adenovirus death protein (ADP) is required for lytic infection of human lymphocytes. J Virol. 2014; 88 (2): 903-912.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/