J Med Discov (2020); 5(2):jmd20033; DOI:10.24262/jmd.5.2.20033; Received April 03rd, 2020, Revised May 8th, 2020, Accepted May 21st, 2020, Published May 29th, 2020.
Spontaneous rectus sheath hematoma (SRSH): a rare cause of acute abdomen in specific patient populations
Harith Alataby1, Jaraad Dattadeen1, Jay Nfonoyim1
1Richmond university medical center, Staten Island, New York, USA, 10310.
* Correspondence:Harith Adnan Alataby.Richmond university medical center, Staten Island, New York, USA, 10310.Email address: harith_adnan_89@yahoo.com
Abstract
Abstract In our case, we are presenting large rectus sheath hematoma in an elderly female with multiple risk factors (Diabetes Mellitus on insulin, asthma, previous abdominal surgery, and obesity). It is vital to keep in mind this differential diagnosis for abdominal pain because it is fatal in some cases. CT Abdomen and pelvis with and without contrast showed large right rectus sheath hematoma approximately 9.2 x 4.2 x 30 cm without active feeding vessel identification. The patient was observed four days in the hospital with monitoring for hypotension and anemia with pain control then discharged with outpatient follow up with PCP and general surgeon.
Keywords: large rectus sheath hematoma, multiple risk factor, case report
Introduction
Rectus sheath hematoma (RSH) can be defined as the accumulation of blood within the sheath of the rectus abdominus muscle located in the abdominal wall. (1-2)
RSH is most common in females around the age of fifty, with the most common triggering factor as acute paroxysmal coughing.
RSH can be differentiated into two types, spontaneous and non-spontaneous. If it occurs in patients without any history of trauma, then it is deemed spontaneous. (3-6-7)
We are presenting this case for the rarity of such an entity and emphasizing the need to consider this entity in the initial differential diagnoses of patients presenting with abdominal pain.
Case Report
64-year-old obese female with PMHx of DM on insulin, HTN, asthma, fatty liver, diverticulitis with history of ruptured diverticulitis and colostomy closure surgery, repaired abdominal hernia, bilateral Knee replacement surgery, who presents with one-day history of right side abdominal pain which is preceded with multiple bouts of cough for the last one week.
The patient denies fevers, chills, nausea, emesis, changes in bowel/bladder habits. Pt is Ex-smoker and quite 25 years ago and denied EtOH use. There was no history of any trauma. Abdominal exam was positive for asymmetry with more prominent on the right side, tenderness especially in the right lower abdomen, rebound tenderness is positive, percussion induced pain is positive, some spots of insulin sc injection sites, and large ecchymosis right flank (Grey-turner’s sign).
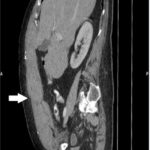
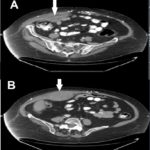
The vital signs were within the normal range. Laboratory wise, hemoglobin initially was 11.9, then drop to 10.6 and stabilized around that value, Mild Elevated Liver function, and lactic acid was 3.3, then normalized during the hospital stay, all other blood tests were within the normal range. Urgently abdomen and pelvis CT scan and CT Angiogram are performed, and the impression was positive for large right rectus sheath hematoma approximately 9.2 x 4.2 x 30 cm, (Figure1), with no feeding vessel identified (Figure 2).
Figure 1 (A, B, C); Abdomen and pelvis CT scan show right rectus sheath hematoma (White arrow), approximately 9.2 x 4.2 x 30 cm.
Figure 2 (A, B): Abdomen and pelvis CT angiogram shows rectal sheath hematoma without feeding vessel identified (White arrow).
The abdominal pain was well controlled by tramadol and Tylenol, and the patient placed under close monitor for hypotension, dropping of hemoglobin, serial abdominal examination for four days in the hospital, she was quite stable clinically, the discharged with outpatient follow up with PCP and general surgeon.
Discussion
RSH designates a collection of blood in the rectus sheath secondary to damage of blood vessels passing through it or injury to the muscle itself.
The causes can be linked to any type of trauma or surgical procedures involving the abdomen, trocar site injury during laparoscopy, drug injections that require subcutaneous administration such as insulin, any anticoagulation, coughing or physical exercise. Medical causes such as hematological diseases, hypertension, or pregnancy can also contribute. The spontaneous occurrence of this process rarely occurs. (3)
Although rare, it is a cause for acute abdominal pain with no other explanation and usually presents with ecchymosis and abdominal wall tenderness. As a result, if SRSH is not considered as a differential for a patient presenting with an acute abdomen, then an unnecessary laparotomy will be performed, resulting in undesired and avoidable side effects. [1-4].
For symptoms, the most commonly reported is Abdominal pain (84–97% of cases). Other findings include an abdominal wall mass (63–92%), positive abdominal guarding (49%), nausea (23%), ecchymosis (21%), and vomiting (15%). The pain can be described as sharp, non-radiating, unilateral, and continuous. As with our patient, the pain is usually exacerbated by movement. Occasionally an abdominal mass may be palpated, which can be non-pulsating but tender. To help differentiate between the abdominal wall and intra-abdominal wall origins, Carnett’s sign (an increased tenderness after tensing the abdominal muscles via lifting the head and shoulders or raising both legs with straight knees) can be used.
Additionally, depending on the site and size of the hematoma, peritoneal irritation signs and symptoms may be present and would vary with intensity. If there is considerable blood loss, hypotension and tachycardia may be present. (7)
Ecchymoses can be seen in the flanks or periumbilical areas, especially late in the course, and are referred to as Gray Turner’s and Cullen’s sign, respectively (6).
Diagnostic testing includes Ultrasonography as an initial test because of its portability and easy accessibility, and noncontract CT scan as a more specific and sensitive choice. Based on the CT findings, RSH can be classified into three subtypes. Type I RSH is small and confined within the rectus muscle without crossing the midline or dissecting fascial planes. Type II remains limited to the rectus muscle but can pass the midline or dissect the transversalis fascia plane. Type III is more extensive, with evidence of hemoperitoneum and/or blood within the perivesical space (or cave of Retzius). As a result, diagnosis of RSH requires both evidence from history and physical exam findings, coupled with supportive imagery. Additionally, coagulation studies should be checked to rule out any undiagnosed hematologic disorder contributing to RSH. As with any other type of bleeding, serial hemoglobin or hematocrit levels should also be obtained. (6-7).
In terms of management, RSH treatment should mostly be conservative such as analgesia, compression at the site, ice pack application, bed rest, and fluid resuscitation. It is essential to discontinue any anticoagulation that the patient may be taking depending on the type of RSH found on CT, using clinical judgment as a guideline. (4-5)
Type one and two may require hospitalization for around five days or if symptoms have improved and rarely need any blood transfusion. For type three, blood transfusions are often required. Invasive therapy is seldom required for type one and type two unless if the patient is hemodynamic instability. Type three RSH that does not respond to fluid resuscitation and FFP, surgical intervention will be indicated which, consists of the evacuation of the clotted hematoma and ligation or cauterization of the bleeding vessel. (4-5) (8)
For large hematomas, digital subtraction angiography and arterial embolization were proven to be safe and effective. (9).
Serious complications of RSH include infection, hypovolemic shock, myonecrosis, abdominal compartment syndrome, myocardial infarction, small bowel ileus, small bowel infarction, intraperitoneal rupture, acute renal failure, and even death. In elderly adults, RSH can become fatal, especially in those with substantial comorbidities (9).
RSH has a reported overall mortality of 4%. Specifically, for iatrogenic RSH, it is 18% but is increased to 25% for those on anticoagulation. Pregnant patients and fetuses have a mortality rate of 13% and 50%, respectively. Therefore, it is essential to have prompt and early diagnosis coupled with proper management of RSH to decrease maternal and perinatal morbidity and mortality rates. (10)
Conclusion
SRSH should be considered as one of the initial differential diagnoses of patients presenting with an acute abdomen. Conservative management with close monitoring of hemoglobin and hematocrit, Blood pressure, abdominal exam series is essential for avoiding unnecessary surgical intervention and preventing severe complications.
Conflict of interest
None
Acknowledgments
None
References
- Gangemi A, Mashbari HN, Bui JT. Obstructive Uropathy because of a Large Rectus Sheath Haematoma: A Case Report of Combined Interventional Radiology and Surgical Approach. EJVES short reports. 2017 Jan 1;34:24-7.
- Chong HC, Chai FY, Tan YE, Heng SS, Desa SA. A rare cause of acute abdomen–Spontaneous rectus sheath hematoma. Asian Pacific Journal of Tropical Biomedicine. 2016 Oct 1;6(10):892-5.
- Kapan S, Turhan AN, Alis H, Kalayci MU, Hatipoglu S, Yigitbas H, Aygun E. Rectus sheath hematoma: three case reports. Journal of medical case reports. 2008 Dec;2(1):22.
- Paschou E, Gavriilaki E, Kalaitzoglou A, Mourounoglou M, Sabanis N. An uncommon presentation of spontaneous rectus sheath hematoma with acute kidney injury due to obstructive uropathy and prerenal azotemia. Case reports in emergency medicine. 2014;2014.
- Romic I, Pavlek G, Mance M, Romic M, Moric T. Fatal case of spontaneous rectus sheath hematoma caused by anticoagulant and steroid therapy during hospital admission. Visceral medicine. 2018;34(3):222-4.
- Alla VM, Karnam SM, Kaushik M, Porter J. Spontaneous rectus sheath hematoma. Western Journal of Emergency Medicine. 2010 Feb;11(1):76.
- Selma AB, Genese T. Spontaneous Rectus Sheath Hematoma: An Uncommon Cause of Acute Abdominal Pain. The American journal of case reports. 2019;20:163.
- Salemis NS, Gourgiotis S, Karalis G. Diagnostic evaluation and management of patients with rectus sheath hematoma. A retrospective study. International Journal of Surgery. 2010 Jan 1;8(4):290-3.
- Ducatman BS, Ludwig J, Hurt RD. Fatal rectus sheath hematoma. JAMA. 1983 Feb 18;249(7):924-5.
- Pierro A, Cilla S, Modugno P, Centritto EM, De Filippo CM, Sallustio G. Spontaneous rectus sheath hematoma: the utility of CT angiography. Radiology case reports. 2018 Apr 1;13(2):328-32.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/