J Med Discov (2019); 4(3):jmd19015; DOI:10.24262/jmd.4.3.19015; Received May 22nd, 2019, Revised July 05th, 2019, Accepted July 30th, 2019, Published August 13th, 2019.
Suppurative (septic) Thrombophlebitis of the Internal Jugular Vein in Hemodialysis patient
Ali A. Mahdi1,*, Omar S. Mahmood1, Bashar Al hemyari2, Sahar E. Mohammadi2
1Sutter Institute for Medical Research,2825 Capitol Ave, Sacramento, CA, 95816
2University of California Riverside School of Medicine, 4445 Magnolia Ave, GME Office, Riverside, CA 92501
* Correspondence: Ali A. Mahdi, Sutter Institute for Medical Research, 6430 Verner Av., Apt 32, Sacramento, CA, 95841. Email: ali_alrawi_2004_1987@yahoo.com
Abstract
Catheter-related Suppurative (Septic) Thrombophlebitis is a rare life-threatening complication that requires early recognition and starts of appropriate therapy. The diagnosis is based on bacteremia with radiographic evidence of thrombosis at the site of the catheter. There are no randomized studies to guide the optimal choice or duration of antibiotics, use of anticoagulants, thrombolytic agents, or excision of the involved vessel, but the available evidence suggests that the administration of heparin should be considered early in the management of patients with septic thrombophlebitis. Here we present a case of Staphylococcus Aureus Septic Thrombophlebitis of the left Internal Jugular vein in End-Stage Renal Disease (ESRD) patient on hemodialysis that was successfully treated with prolonged antibiotic and anticoagulation therapy.
Keywords: Hemodialysis , Catheter-related Suppurative (Septic) Thrombophlebitis, anticoagulation therapy.
Background
Staphylococcus Aureus Bloodstream Infection (BSI) is a common and significant cause of morbidity and mortality in hemodialysis patients. Most of those infections (83%) were related to vascular catheters[1].
Catheter-related Suppurative (Septic) Thrombophlebitis is a rare life-threatening complication that requires early recognition and starts of appropriate therapy. Long-term indwelling catheters are known to independently increase the risk of venous thrombosis because the insertion can cause damage to the vessel wall and activation of the intrinsic coagulation pathway[2]. On the other hand, septicemia has been shown to be associated with a ≥3-fold increase in the risk of development of deep venous thrombosis[3].
The diagnosis is typically suspected in patients with persistent central line-associated bloodstream infection (CLABSI) after 72 hours of appropriate antimicrobial therapy[4]. The diagnosis is based on bacteremia with radiographic evidence of thrombosis at the site of the catheter[5]
Here we present a case of Staphylococcus Aureus Septic Thrombophlebitis of the left Internal Jugular vein in End Stage Renal Disease (ESRD) patient on hemodialysis that was successfully treated with prolonged antibiotic and anticoagulation therapy.
Case Presentation
53 years old Male with End Stage Renal Disease Presented to the Emergency with left-sided chest pain since waking up in the morning, squeezing in nature, radiating to the left neck, progressive throughout the day, Pain was relieved temporarily with home Nitroglycerine, associated with fever, chills, and malaise.
The fever started 3 days prior to his presentation and was Partially relieved by Tylenol which enabled him to attend the scheduled dialysis sessions. One night prior to presentation, his fever returned and had persisted since. He denies shortness of breath, cough, palpitations, nausea, vomiting, dysuria, headache, numbness, or weakness
Past Medical History: Insulin Dependent Diabetes mellitus, End Stage Renal Disease on Hemodialysis, Myocardial infarction, peripheral neuropathy, Transient Ischemic Attack, endocarditis.
Past surgical history: amputations of left ring and middle fingers and all right toes secondary to Diabetes mellitus (DM), amputation of right 5th digit, Coronary Artery Bypass Grafting (CABG), Right lower Extremity bypass, Appendectomy.
Social History: Alcohol use (Occasional), Drug use (In Recovery).
On Physical Examination, the patient was alert, awake, oriented to person /place/time. On neck examination, there was no Jugular vein distension (JVD) or Lymphadenopathy (LAP), a tunneled catheter well placed in the left Internal Jugular vein with some overlying erythema and tenderness but no discharge.
Heart and lungs examination were normal.
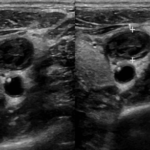
Fig. 1 Left internal jugular vein thrombus
Investigations
- ECG (Electrocardiogram): normal
- Cardiac Enzymes: normal
- Chest X-Ray: normal
- CTA (Computed tomography angiography) chest: normal
- Transthoracic Echocardiogram (TTE): negative
- Complete Blood Count and Differential: normal WBC count, normocytic anemia.
- Serum Electrolytes: normal Potassium, Hyponatremia (131 mmol/L)
- Metabolic Panel: eGFR (9 mL/min per 1.73 m2 ) , BUN (36 mg/dL), Creatinine (7.46mg/dL) , Glucose (228 mg/dL)
- Elevated ESR (42 mm/hr.) and Procalcitonin (5.99 ng/mL)
- Blood culture and sensitivity: Methicillin Sensitive Staphylococcus Aureus (MSSA) sensitive to Nafcillin.
- The HD catheter was removed, and the tip culture grew MSSA. Fungal culture, fungitell, T12 candida all negative.
- Transesophageal Echocardiogram (TEE) : negative
- Ultrasonography (US) of the left internal jugular vein: revealed an infected thrombus. (figure 1,2)
Differential Diagnosis
- Acute Coronary Syndrome ruled out with EKG and cardiac enzymes
- Pericarditis: ruled out with EKG and echo
- Pneumonia: ruled out with chest X-ray
- Pulmonary Embolism: ruled out with CTA chest
- Infective Endocarditis: ruled out with negative Transthoracic Echocardiogram (TTE) and later on by the negative Transesophageal Echocardiogram (TEE)
Treatment
According to the Guidelines for the Diagnosis and Management of Intravascular Catheter-Related Infections published by the Infectious Diseases Society of America[5], suspected CRBSI among patients who are undergoing hemodialysis (HD) with tunneled catheters is an indication to start immediate empiric antibiotics once blood culture samples are obtained. In our case, the blood culture grew MSSA sensitive to Nafcillin. Hence the empiric antibiotics were switched to IV Nafcillin.
On day five of the admission, the patient had a persistent fever and bacteremia despite antibiotic treatment, which (according to the guidelines[5]) warrants the removal of the Central Venous Catheter. Culture of the catheter tip grew MSSA. Further evaluation for endocarditis and thrombosis were performed. TEE was negative, but the Ultrasound of the left Internal Jugular vein revealed an infected thrombus which (along with bacteremia) satisfies the definition for Septic Thrombophlebitis.
There are no randomized studies to guide the optimal choice or duration of antibiotics, use of anticoagulants, thrombolytic agents, or excision of the involved vessel, but the available evidence suggests that the administration of heparin should be considered early in the management of patients with septic thrombophlebitis [6-8].
Accordingly, we started our patient on Heparin drip in addition to the antibiotic, the patient’s fever subsides and the heparin was switched to Apixaban upon discharge.
After six weeks of continued antibiotic and anticoagulation treatment, the patient was seen in the outpatient clinic with resolved thrombus and the blood culture turned negative.
A new Hemodialysis catheter was placed after the blood culture turned negative.
Fig. 2 Left internal jugular vein thrombus
Discussion
The main challenge in the management of this case was the course of action to be followed after the diagnosis of Septic Thrombophlebitis was established, The guideline[5] recommends extended antibiotic treatment for a minimum of 3-4 weeks. Limits the surgical excision option to patients with purulent superficial veins or patients in whom the infection extends beyond the vessel wall. And mentions that the role of heparin in this setting is “unresolved” due to the lack of data from comparative trials that are required to draw definitive conclusions. The bulk of the evidence comes from case series and case reports. Falagas et al. performed a systematic review to evaluate the role of heparin in this settting[6]. In this paper, fourteen articles describing the cases of 216 cases with septic thrombophlebitis were included for evaluation in this systematic review. The results of this review suggest that the use of heparin in combination with antibiotics is associated with low mortality in patients with Septic Thrombophlebitis. In addition, adverse effects related to heparin were limited in the reported literature.
In another retrospective study, Wilson et al.[4] evaluated 128 patients with Septic Thrombophlebitis to assess the difference of outcome in response to various treatments. In the results, One of the significant findings mentions that not receiving anticoagulant therapy was a predictor of failure of treatment (OR, 0.24; 95% CI, 0.11-0.54; P < .001). The final conclusion of this study recommends prolonged intravascular antimicrobial therapy and administration of anticoagulation therapy early in the management of Septic Thrombophlebitis.
Learning Points
- Chest pain could be the presenting symptom of septic thrombophlebitis of the Internal Jugular vein and mimic possible endocarditis or acute coronary syndrome.
- Persistent fever and bacteremia among patients undergoing hemodialysis with tunneled catheter despite appropriate antibiotic treatment require further evaluation for the underlying focus of infection (septic thrombosis or endocarditis).
- The patient`s improvement started after initiating heparin, which emphasizes their potential role to dissolve and eliminate the source of infection, however, there is a need for stronger evidence to establish their definite role in the guideline.
- The provision of lower-risk vascular access, such as arteriovenous fistulae, and reduced use of intravascular catheters should be priorities in all hemodialysis units. Where alternative vascular access cannot be established, interventions to reduce the risk of catheter-related infections should be implemented to reduce morbidity and mortality in this vulnerable patient group[1].
Conflict of interest
None
Acknowledgments
None
References
1. Fitzgerald SF, O’Gorman J, Morris-Downes MM, et al. A 12-year review of Staphylococcus aureus bloodstream infections in haemodialysis patients: more work to be done. J Hosp Infect. 2011;79(3):218-221.
2. Saber W, Moua T, Williams EC, et al. Risk factors for catheter-related thrombosis (CRT) in cancer patients: a patient-level data (IPD) meta-analysis of clinical trials and prospective studies. J Thromb Haemost. 2011;9(2):312-319.
3. Mejer N, Westh H, Schonheyder HC, et al. Increased risk of venous thromboembolism within the first year after Staphylococcus aureus bacteraemia: a nationwide observational matched cohort study. J Intern Med. 2014;275(4):387-397.
4. Wilson Dib R, Chaftari AM, Hachem RY, Yuan Y, Dandachi D, Raad, II. Catheter-Related Staphylococcus aureus Bacteremia and Septic Thrombosis: The Role of Anticoagulation Therapy and Duration of Intravenous Antibiotic Therapy. Open Forum Infect Dis. 2018;5(10):ofy249.
5. Mermel LA, Allon M, Bouza E, et al. Clinical practice guidelines for the diagnosis and management of intravascular catheter-related infection: 2009 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;49(1):1-45.
6. Falagas ME, Vardakas KZ, Athanasiou S. Intravenous heparin in combination with antibiotics for the treatment of deep vein septic thrombophlebitis: a systematic review. Eur J Pharmacol. 2007;557(2-3):93-98.
7. Tovi F, Fliss DM, Noyek AM. Septic internal jugular vein thrombosis. J Otolaryngol. 1993;22(6):415-420.
8. Volkow P, Cornejo-Juarez P, Arizpe-Bravo AB, Garcia-Mendez J, Baltazares-Lipp E, Perez-Padilla R. Catheter-related septic thrombophlebitis of the great central veins successfully treated with low-dose streptokinase thrombolysis and antimicrobials. Thromb J. 2005;3:11.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/