J Med Discov (2018); 3(2):jmd18020; DOI:10.24262/jmd.3.2.18020; Received April 23rd, 2018, Revised May 11th, 2018, Accepted May 18th, 2018, Published June 20th, 2018.
Long Acting Reversible Contraception (LARC) among young women and adolescents
Rasha Azeez Hammood Al-Lami1, Ammar Mohammed Ali Abdulhussein Algburi2
1Department of Preventive Medicine and Community Health, University of Texas Medical Branch, Galveston, TX.
2Department of Internal Medicine, Al-Yarmouk Teaching Hospital, Baghdad, Iraq.
* Correspondence:Address to Rasha Al-Lami, M.D., Department of Preventive Medicine and Community Health, University of Texas Medical Branch, 301 University Blvd, Galveston TX 77555 (raallami@utmb.edu, +1 409 256 3310).
Abstract
long-acting reversible contraceptives (LARC) such as intrauterine devices (IUDs) and subdermal implants remain the most effective methods of contraception for young women (age 19-24 years) and teenagers or adolescents (age 13-19); however, most young women and adolescents continue to use less reliable methods of contraception rendering them very susceptible to be pregnant and to carry the risk of long lasting health, social and economic burden of teen pregnancies. United States continue to have the highest level of teenagers’ pregnancies in comparison to developed countries. Moreover, young women uptake and awareness of LARC effective methods of contraception is low at school-based clinics which is the most available and suitable clinic setting to this age group. Further research should be directed to find policies that can enhance LARC availability and uptake in such settings and provide appropriate counselling to increase LARC uptake by young women. We used Medline-PubMed to review any type of studies that addressed LARC advantages, disadvantages, teen pregnancy rate, consequences and cost burden, clinics LARC uptake and awareness of young women and female teenagers (age 13-24yeras). Few electronic sources cited in this review were also searched manually.
Keywords: Long acting reversible contraception (LARC); young women; female adolescent
Introduction
Although the teenage pregnancy rate has decreased over the past decade, the U.S. still has the highest teen birth rate among developed countries. 1 The most effective method of contraception for adolescent girls is long-acting reversible (LARC) such as intrauterine devices (IUDs) and subdermal implants. 2
Review
Effectiveness and advantages
LARC including intrauterine device (IUD) and subdermal implant are the most effective form of contraception, with failure rate of only 0.2 % for levonorgestrel IUD, 0.6-0.8% for copper IUD and <1% for the implant in comparison with first year failure rate of 15% for male condoms, 6% for Depo-Provera and 8% for oral contraceptive pills. 3
LARC methods have the advantage of being independent of compliance unlike strict pills-taking regimen and frequent healthcare visit need for injections. LARC also provide long-lasting contraception that could maintain contraception for years and most importantly it does not include the component of Estrogen that is proved to cause many hormonal related health problems including breast cancer. 3,4
LARC uptake
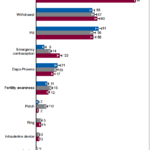
LARC usage by young women and adolescents in the United States remains low. Although the percentages of those used implant increased from the period of 2006-2010 to the period 2010-2015 but remains very low in comparison to other modes of contraception. Fig.1. 2.5% of teen females reported using IUD for the period 2006-2010 compared to 2.8% of them used IUD in 2011-2015, 0.6% of teenage females used implants for the period 2006-2010 compared to 3% of them used implants in 2011-2015, with the least effective contraception methods, condoms and withdrawal, being the most frequently used contraceptive measures in female teenagers (97.4% of teen females reported using condoms and 59.7% reported using withdrawal). 5 Additionally, an article that used the 2006-2010 National Survey of Family Growth (NSFG) data found that LARC use has increased only in women 18 years and older in comparison to women less than 18 years of age. 6
Figure 1. Methods of contraception used among females aged 15-19 who ever had sexual intercourse. United States, 2002, 2006-2010 and 2011-2-015. 5
Teen pregnancies and the need for effective control
Although the teenage pregnancy rates have decreased recently in comparison to 1980s, the U.S. still records the highest teenage pregnancy rate among developed countries worldwide. It is documented that in 2010, the teens pregnancy rate in U.S. was 57.4 per 1000 women, the birth rate 34.4 per 1000 women, and abortion rate 14.7 per 1000 women in comparison to 1980s and 1990s when the teenage pregnancy rate was 116.9 per 1000 women, the birth rate 61.8 per 1000 women, and the abortion rate 43.5 per 1000 women. It is also estimated that 3 in each10 teens will become pregnant before the age of 20, resulting in nearly 750,000 pregnancies each year with more than 80% of which are unplanned. 7
An effective form of contraception is required in this age group and mere educational programs cannot be sufficient. In a systematic review that assessed pregnancy prevention programs, including sex education classes, school-based clinics, family planning clinics, and community based programs, effect on delay in initiation of sexual intercourse, consistent use of any form of birth control, or avoidance of unintended primary pregnancy in 22 published and unpublished randomized controlled trials of adolescents (ages 11 to 18 years) in North America, Australia, New Zealand, or Europe found that these interventions did not delay initiation of sexual intercourse in young women, did not improve use of birth control by young women at every intercourse or at last intercourse and did not reduce pregnancy rates in young women. It also found that only four abstinence programs and one school-based sex education program were associated with an increase in number of pregnancies among partners of young male participants. 8
Impact of unplanned pregnancies on young women and teenagers
Reducing teens birth can have public and personal benefits. In 2010, teen pregnancy and childbirth accounted for at least $9.4 billion in costs to U.S. taxpayers for increased health care and foster care, increased incarceration rates among children of teen parents, and lost tax revenue because of lower educational attainment and income among teen mothers. 9
The individualized effect of early pregnancy can exert potential harm in the future. A woman who has a baby in her teens is significantly more likely to have lower educational levels and income in her adulthood in comparison to her non-childbearing peers who did not have teen birth. 5 Moreover, this effect could extend to further generations. A study conducted on 17,115 women between the ages of 14-19 years concluded that having an older sister who gave birth while she was teen was significantly associated with her younger sibling having teen pregnancy. In addition, teen mothers’ daughters were more likely to be pregnant during their teenage period compared to daughters of mothers who had their first pregnancy after the age of 19 years. 10 Although this study was conducted in one of Canada provinces, U.S. population shared a lot of demographics with Canada’s population. In another study conducted on 318 girls age 12-18 with long term follow up of their offspring to the age of 14 years concluded that early sexual maturation of the children of teen mothers was associated with early sexual experience in daughters, and could be a pathway for the inter-generational transfer of risk for teenage pregnancy among daughters of teenage mothers. 11
In regards to teens pregnancy health consequences, teenage mothers’ children frequently born pre-term, with lower birth weight, and higher neonatal mortality. 12 Moreover, the risk of unplanned pregnancy could be enhanced by the level of the stress these young women experience during their adolescence which is positively associated with high sexual behaviors rendering these young women susceptible to unplanned pregnancy. 13
LARC awareness among young women and teenage females
Increasing young women awareness of LARC is very important to achieve higher uptake of effective methods of contraception especially those young women have little awareness of the availability and effectiveness of LARC and they are always being misled by media or personal experience of a close peer. 14 The contraception prospective cohort CHOICE project that was done in St. Louis, MO. aimed to remove financial barriers, promote the use of LARC and evaluate the use, continuation and satisfaction among a cohort of 10,000 women between the ages 14-45 years old women who wanted to avoid pregnancy for at least one year and initiating a new form of reversible contraception who were split into LARC-users and non-LARC-users. Through this project, it has shown that once financial barriers were removed and LARC methods were introduced to all potential participants as a first-line contraceptive option, almost two thirds of the participants chose LARC. 15 Another study that evaluated the acceptance of LARC among adolescents using CHOICE project data concluded that LARC use is acceptable and common among adolescents (age 14-20 years) enrolled in the project, with the younger group (age 14-17 years) being most interested in the implant. 16 This hope of young females’ adherence and desire to use LARC is further supported by the finding of another study; the study used CHOICE project data to test the continuation of LARC usage in young females age 14-25 years and found that 12 months continuation of LARC was almost 75% for all ages with young females age 14-19 years had slightly lower continuation rate of 81% in comparison to older female participants continuation rate of 85%. Added to that, young females age 14-19 had lower continuation rate of 44% for non-LARC methods. 17
Improving school-based clinics with proper counseling and guidance on how to use LARC to young females is a necessity to prevent unintended pregnancies and improve quality of life in these females. A cross sectional study conducted on 13-19 years old female participants from 2 urban school-based clinics in Seattle found that only 50% of these females know that LARC is the most effective method of contraception, 61% believe that insertion of IUD or placing the implant is a simple procedure, 46% believe that LARC can be used only after having a baby, 47% believe LARC would decrease future fertility, almost half of them believe that it should be used only before intercourse and don’t know that IUD can be placed for 5-7 years and almost 30% believe that LARC could protect against HIV with their final conclusion that LARC knowledge and acceptability vary among these adolescents who attended school based health center. 18
Cost of LARC
Although being criticized for cost effectiveness, a study was done using three-state economic model on 1000 women age 20-29 years for 5 years duration concluded that LARC methods become cost neutral with short-acting-reversible contraception (SARC) within 3 years of use with key finding that the two least expensive methods were copper IUD ($304 per women/per year) and Levonorgestrel intrauterine system 20 mcg/24 h ($308) while cost of SARC methods ranged from $432 (injection) to $730 (patch), per women, per year. 19
Further advantages
LARC could also be an effective method of contraception in women with underlying comorbidity. A case series was conducted to test LARC associated complications in patients with cardiovascular disease especially found that Levonorgestrel intrauterine system can be beneficial in this group since it decreases menstrual bleeding by 90% after 6 months of usage and can reduce anemia and heavy menstrual bleeding associated with anti-coagulant use in cardiovascular patients with overall low rate of LARC associated complications in terms of pelvic pain, abnormal vaginal bleeding, PID, endometritis, IUD expulsion, uterine perforation and mood changes. 20
In conclusion, the high efficacy, low rate of complications, relative cost effectiveness of LARC necessitate its use in most vulnerable individuals such as young females age 13-24 years to prevent unplanned teen pregnancies that could impact a heavy toll on the long run. Given the low awareness of this age group and lack of guidance and counselling by school-based clinics, increasing access, uptake and counselling by offering LARC to teenagers in school-based health clinics or in clinics where teenagers congregate frequently (i.e. retail store-based clinics) holds both public health and clinical positive impact in this vulnerable age group.
Conflict of interest
The authors declare that they have no competing interests.
Acknowledgments
None
References
1. Centers for Disease Control and P. Prepregnancy contraceptive use among teens with unintended pregnancies resulting in live births – Pregnancy Risk Assessment Monitoring System (PRAMS), 2004-2008. MMWR Morbidity and mortality weekly report. 2012;61(2):25-29.
2. Committee on Adolescent Health Care Long-Acting Reversible Contraception Working Group TACoOaG. Committee opinion no. 539: adolescents and long-acting reversible contraception: implants and intrauterine devices. Obstetrics and gynecology. 2012;120(4):983-988.
3. Stoddard A, McNicholas C, Peipert JF. Efficacy and safety of long-acting reversible contraception. Drugs. 2011;71(8):969-980.
4. Hilakivi-Clarke L, de Assis S, Warri A. Exposures to synthetic estrogens at different times during the life, and their effect on breast cancer risk. J Mammary Gland Biol Neoplasia. 2013;18(1):25-42.
5. Abma JC, Martinez GM. Sexual Activity and Contraceptive Use Among Teenagers in the United States, 2011-2015. Natl Health Stat Report. 2017(104):1-23.
6. Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007-2009. Fertil Steril. 2012;98(4):893-897.
7. Kathryn K, Stanley H. US Teenage Pregnancies, Births and Abortions: National and State Trends and Trends by Race and Ethnicity. 2010; https://www.guttmacher.org/sites/default/files/report_pdf/ustptrends10.pdf.
8. DiCenso A, Guyatt G, Willan A, Griffith L. Interventions to reduce unintended pregnancies among adolescents: systematic review of randomised controlled trials. Bmj. 2002;324(7351):1426.
9. National Campaign to Prevent Teen and Unplanned Pregnancy. https://powertodecide.org/what-we-do/information/why-it-matters.
10. Wall-Wieler E, Roos LL, Nickel NC. Teenage pregnancy: the impact of maternal adolescent childbearing and older sister’s teenage pregnancy on a younger sister. BMC Pregnancy Childbirth. 2016;16(1):120.
11. De Genna NM, Larkby C, Cornelius MD. Pubertal timing and early sexual intercourse in the offspring of teenage mothers. J Youth Adolesc. 2011;40(10):1315-1328.
12. Chen XK, Wen SW, Fleming N, Demissie K, Rhoads GG, Walker M. Teenage pregnancy and adverse birth outcomes: a large population based retrospective cohort study. Int J Epidemiol. 2007;36(2):368-373.
13. Hall KS, Kusunoki Y, Gatny H, Barber J. Stress symptoms and frequency of sexual intercourse among young women. J Sex Med. 2014;11(8):1982-1990.
14. Teal SB, Romer SE. Awareness of long-acting reversible contraception among teens and young adults. J Adolesc Health. 2013;52(4 Suppl):S35-39.
15. Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203(2):115.e111-117.
16. Mestad R, Secura G, Allsworth JE, Madden T, Zhao Q, Peipert JF. Acceptance of long-acting reversible contraceptive methods by adolescent participants in the Contraceptive CHOICE Project. Contraception. 2011;84(5):493-498.
17. Rosenstock JR, Peipert JF, Madden T, Zhao Q, Secura GM. Continuation of reversible contraception in teenagers and young women. Obstet Gynecol. 2012;120(6):1298-1305.
18. Hoopes AJ, Ahrens KR, Gilmore K, et al. Knowledge and Acceptability of Long-Acting Reversible Contraception Among Adolescent Women Receiving School-Based Primary Care Services. J Prim Care Community Health. 2016;7(3):165-170.
19. Trussell J, Hassan F, Lowin J, Law A, Filonenko A. Achieving cost-neutrality with long-acting reversible contraceptive methods. Contraception. 2015;91(1):49-56.
20. Vu Q, Micks E, McCoy E, Prager S. Efficacy and Safety of Long-Acting Reversible Contraception in Women With Cardiovascular Conditions. Am J Cardiol. 2016;117(2):302-304.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/