J Med Discov (2018); 3(1):jmd17054; DOI:10.24262/jmd.3.1.17054; Received December 12nd, 2017; Revised January 17th, 2018; Accepted February 10th, 2018; Published March 20th, 2018.
Acute Mountain Sickness: Travellers Should Get Enough Information
Dra Susana Domínguez Rovira1
1. Public Health Care Center “17 de Setembre”. El Prat de Llobregat 08020, Barcelona. Spain.
* Correspondence: Dra Susana Domínguez Rovira Public Health Care Center “17 de Setembre”. El Prat de Llobregat 08020, Barcelona. Spain.
E-mail: susanadrovira@gmail.com
Introduction
Acute mountain sickness (AMS), also called soroche, is advised to be prevented before visiting touristic spots at highlands with continuously arising altitudes by the external consultation services. High altitude has generally been defined as an elevation above 2500-3000 meters (approximately 8200-10000 feet). Going to ski in the top of the Pyrenees or the Alps is common and children over two years old are admitted to the cableway that takes you to nearly the top of Teide volcano (3718 m, Canary Islands). Rocky Mountains, Himalayan or Andean Mountain Ranges, once reserved for a few, are becoming popular vacation destinations. In spite of these increased interest, it is unknown whether there is an actual increased awareness among trekkers, and if this awareness is accompanied by a decrease in the prevalence of AMS.[1]
The documented prevalence of AMS varies a lot between 15 and 75% depending on the altitude reached, speed of ascent and individual susceptibility.[2] Surveys in Colorado ski areas revealed an incidence of 25% in both adults and children but the younger individuals have more risk at developing AMS.[3,4]
A prospective on-site study in the Himalayas in 2004 found that 68% of trekkers had received any written/oral information about AMS prior to their departure. Among them 47% suffered symptoms of AMS, which in 50% began at 3000 meters. About one third of the affected ones had acetazolamide with them, but only half of them actually used it. Surprisingly, only 2-16% of all travelers knew that oxygen was a treatment option.[1]
The simplest counseling would be “Do not go there if you want to avoid any risk”. But freedom to discover new horizons must be preserved as well. At this point, medical purposes should focus on preventing AMS and public should become familiar with the signs and symptoms of AMS when ascending at high altitudes and what to do if so.
Causes and Prevention
Statistic studies are now confirming what highlanders observed: “Everyone can experience AMS, regardless of age, gender or physical condition, even if you did not suffer from it on a previous trip”. Nevertheless, pre-acclimatization based on regular exposures to altitude, prior to traveling abroad, could help.
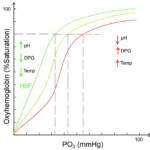
There is a relationship between the prevailing oxygen tension (horizontal axis) and the saturation (oxygen-laden) of the hemoglobin molecule in the blood (vertical axis). As seen in the figure 1, it takes a sigmoidal shape and it is called “hemoglobin binding or dissociation curve”. It is a valuable tool for understanding how our blood carries and releases oxygen. If oxygen partial pressure is high (lung), oxygen will bound to hemoglobin. On the contrary, if oxygen partial pressure is poor (peripheral tissues), hemoglobin releases oxygen (loose binding). The production of biphosphoglycerate (BPG) in red blood cells is an important adaptive mechanism as it decreases the affinity of hemoglobin for oxygen. It will be easier for the oxygen to unbind and be distributed into tissues. Thus, BPG moves on the curve to the right. Acidity or heat would also provoke the same lateral shift. When a healthy person flies from sea level to high altitude, tissue oxygenation decreases. After hours, BPG arises and so oxygenation of tissues can recover. This situation reverses when this individual gets back to sea level. Regular aerobic training increases intraerythrocytic BPG helping acclimatization.
Fig 1. Schematic curve of oxygen saturation.
Pregnancy might not be the most appropriate time to sleep at altitudes above 3600 meters (12000 feet). First of all, changes at barometric pressure can induce premature labor. Moreover, fetus rely on the oxygen circulating through the mother blood stream. Their specific hemoglobin, fetal hemoglobin (Hb F), has a stronger affinity with oxygen than adult hemoglobin (Hb A) and this way, it sucks out the oxygen of the placenta. After birth, Hb F levels fall down whereas Hb A levels heighten. Hb A is a better deliverer of oxygen to tissues. Hb F may persist along the first 6 to twelve months of life, causing a left shift on the dissociation curve (tight binding, strong affinity). That means, even when oxygen at blood is quite low, it will be difficult to be delivered to tissues.Transient hypoxia may cause long-term sequelae on the fetus and infants. Besides, AMS in children under two years old might be difficult to diagnose. Todlers may become fussy or lose coordination while stepping.
Complications of diabetes may be triggered by AMS and treatment could be harder, so people with diabetes need to be aware of it. People with anemia, intercurrent infections, obesity, heart or lung disease should take clear advice before travelling to highlands.
Changes on cerebral blood flow because of vasomotor adaptations put cortex on a situation of increased vulnerability. Since retina of the eye has a great requirement of oxygen, vision is the first sense altered with the lack of it.[5] In acute hypoxia, severe reduction of arterial oxygen saturation decreases a person´s capacity for mental concentration, fine motor coordination, and leads to faulty judgement and impaired muscular function.[6] Nowadays, aged people also travel around the world and dare to climb mountains. Apparently, healthy aged subjects may adapt fairly well when changes are undertaken slowly, whereas some others may experience alterations in sensory, motor and mental function (attention span, short-term memory, decision making) which must be taken into account in every particular case. Residual neurobehavioral impairment after returning to lower elevations has also been reported.[5] Therefore, medical supervision and precise instructions previous to journey are higly recommended to aged persons.
The very first advice to give everyone is a slow ascent, assuming no more than 400-600 meters (1313 feet) a day is desirable to prevent AMS.[6] Opiate pain medications must be eluded. Hydrating with abundant water and avoiding alcohol might help acclimatization as well.
Regular mountaineers or alpinists carefully and gradually ascend up high altitudes, but less experienced travelers fly straight ahead from sea level to a higher town (for instance, Cusco in Peru, 3399 m or Lhasa in Tibet, 3656 m) and then immediately drive to the mountains to hike. Instead, the recommendation would be to rest for a day or two for acclimatization. This is the main reason why visiting in just 2 hours to Tatio Geysers (4320 m) should be postponed to the last day when visiting Atacama Desert and staying at San Pedro de Atacama (2408 m).
Extenuating exercise or fatty meals will kidnap blood flow at muscles or intestines. Instead, people should better try first short walks, dine lightly and sleep well. However, if people insist on starting activities, a good alternative for the second day might be a day trip to a higher altitude and then return to a lower altitude to sleep.[6]
Oxygen concentration in the air is pretty stable, around 20.95%, in the air. What comes down when climbing up a mountain is not the volume of the air that we inhale but the pressure that our atmosphere infringes above us. And so do all the atmospheric gases. As a result the partial pressure of oxygen, the amount of molecules of oxygen contained in the same inhaled volume will be lower (hypobaric hypoxia).
The proportion of oxygen in the air only starts changing above 100 kilometers high. On the contrary, the number of molecules of air (and the molecules of oxygen as well) per unit of volume does decrease. The phenomenon is not linear. For every 1000 meters we go up we lose around 10% of oxygen molecules during the first 5000 meters. Then, from this point, changes occur softly so that at the altitude of 10000 meters we would have lost 69% of the molecules, but we still have oxygen up there. Barometric pressure not only decreases as one moves up to higher altitudes but also when one moves towards the poles.[6]
Due to this reason, we feel out of breath even during light exercise, or bending down to pick something up on the floor, or holding breath to take a picture, eating or talking. We will feel lightheaded, a bit drowsy or confused. We find difficulties to fall asleep or might even wake up several times all along the night. People explain their sleep was not restful. Headache, poor appetite or vomiting may occur first 6 to 12 hours and usually disappear or improve within 1-2 days if there is no further ascent.
The equations might slightly change with temperature and humidity. Temperature usually decreases at night. Thus, air density arises, joins the molecules and oxygen availability improves. But intense cold will increase thermogenesis (base metabolic rate) needed to survive, and thus increasing oxygen combustion. Humidity makes air become less dense, and oxygen pressure mildly decreases as air passes through the respiratory tract. Water vapor is always present in the air in varying amounts. The amount of water vapor that the air can hold depends on the temperature of the air.
The warmer the air is, the more water vapor can include. The mean monthly relative humidity over the year in Cusco (Peru) is 55% but it reaches an average annual percentage of 69% in Lhasa (Tibet). On average, August is the least humid month in Cusco but it is the most humid month in Lhasa. Because of the temperature gradient, humidity decreases rapidly with altitude. During the day, especially on a sunny day, water vaporizes from forests and lakes. At night, temperature decreseases and water vapor falls down the soil. All in all, high altitude stress is primarily due to hypoxia of low atmospheric pressure, but dry air, intense solar radiation, high winds (they all intensify dehydration), extreme cold and exercise (both elevate oxygen demands) do contribute to AMS. It is essential to bear in mind that appropriate protection can be the key to override the effects of some of these variables. Enough water and suitable warm clothes are always reinforced.[6,7]
We have different tools to detect and quantify severity of AMS. The simplest instrument is the “clinical functional score” (CFS) because it relies on a single question and emphasizes functional limitations resulting from AMS (ordinal scale 0-3). The Lake Louise Questionnaire Score (LLQS) will be used to assess the severity of AMS in those travelers reporting moderate to severe limitations in activities of daily living (CFS>=2).[7]
AMS is a clinical diagnosis in the context of ascending at high altitudes. Physical examination is usually normal. No blood or imaging test is needed. Supplemental oxygen through a nasal cannula can be used as a diagnostic “Test” for AMS and will act as a therapy. Resting, painkillers and hydration will complete the treatment. Similarly, descending will increase oxygen supplies and help recovering from the clinical situation.[8]
Complications and Treatment
Exposure to altitude will potentiate erythropoietin production leading progressively to polycythemia within hours. In addition, staying at the same high altitude, plasma volume decreases during the first 1-2 weeks, which in turn could contribute as well to hindering fluent blood circulation. Hiperviscosity is associated with declining oxygen transport and peripheral extraction. Besides, highlands have usually low humidity and dehydration. That is why increasing liquid or water ingestion is highly encouraged. The high altitude renal syndrome (HARS) comprises, apart from polycythemia, hyperuricemia, systemic hypertension and microalbuminuria. Policythemia might be especially important when high altitudes combine with exposure to heavy metals that can also stimulate erythropoiesis, such as cobalt and nickel, as seen in mining communities,such as Chuquicamata (2870 meters high, Chile ) or North American Rockies.[9]
In less than 1% of cases reported, symptoms of AMS can progress to high altitude pulmonary edema (HAPE) or cerebral edema (HACE), two life-threatening conditions marked either by loss of coordination, wobbly gait (ataxia), confusion or increasing cough and difficulty to breath (dyspnea). Subclinical HAPE is far more frequent than suspected during even modest climbs of average effort, especially if lung size is normal or low. Cremona et al suggested that three of every four healthy recreational climbers may experience some fluid accumulation in the lung shorty after a modest ascent that resolves spontaneously.[10] HAPE is highly correlated with acute pulmonary hypertension (and reduced cardiac outputs). In contrast to systemic blood vessels which dilate in response to hypoxia, the pulmonary blood vessels constrict.[11] HAPE presents within 2-5 days of arrival at high altitude. It is rarely observed below altitudes of 2500-3000 meters and after one week of acclimatization. It is probably due to the fact of adaptive vascular remodeling.[6] Cough worsens and dyspnea appears even at rest. Orthopnea may occur. Gurgling in the chest and pink frothy sputum (alveolar hemorrhage) indicates advanced cases. As the event progresses, cyanosis, tachypnea, tachycardia and elevated body temperature take place. Rales are discrete initially and located over the middle lung fields. It may lead to misdiagnosing pneumonia, as it happened to be described in the last century.[12]
There are several mechanisms responsible for pulmonary hypertension. The first is heterogeneous pulmonary vasoconstriction causing regional overperfusion of capillaries in areas of low arterial vasoconstriction. This causes damage to the capillary walls and subsidiary alveolar hemorrhage. The second is hypoxic constriction occurring at the level of the pulmonary veins, increasing the resistance downstream of the region of fluid filtration. Another mechanism that may contribute to HAPE is a diminished capacity for alveolar fluid re-absorption.[13]
Researchers in the past decade have found that accentuated pulmonary hypertension on ascend (as seen while vigorous exercise) contribute to HAPE. On the contrary, resting while acclimatization and minimizing the pulmonary hypertension would prevent HAPE. Bartsch et al used a calcium channel blocker (nifedipine) on a slow-release formulation to prevent HAPE. However, the general use of this drug is not advocated because of its potentially harmful effects. It should only be considered when the most essential preventive measure, slow ascent, has failed in previous ascents. [14,15]
Acetazolamide is a carbonic anhydrase inhibitor and is indeed effective in AMS (125 mg twice daily, starting the night before the planned ascent and continue until descent) but further research is needed to determine its efficacy in HAPE. It can be used either for prevention (if rapid ascent is inevitable as in certain flights to high towns) or amelioration of AMS in adults and children. Its beneficial effect relies on its respiratory stimulant effect.[6] The guideline dose for children is 2,5 mg/kg orally every 12 hours (maximum 125mg).
Inhaled beta-2-receptor agonists (salmeterol) not only decreases incidence of pulmonary edema, but also attenuates AMS.[16] Yet, they are not generally recommended for the prophylaxis of HAPE due to a lack of studies and side effects at superior doses.
Corticosteroids activate nitric oxide synthase. Dexamethasone seems to be effective in preventing HAPE in susceptible adults when taken one day prior to ascend but the minimal effective dose is not known yet Dexamethasone should be given (8mg initially followed by 4 mg every 6 hours) when HACE is diagnosed, apart from oxygen therapy and descending.[7]
Once HAPE is suspected or diagnosed, immediate improvement of oxygenation either by supplemental oxygen or hyperbaric chamber is the treatment of choice. Shock and death can occur if the symptoms are not recognized and treated. Rapid descent is imperative when sojourning in a remote area. If it takes few days to reach lower altitude, treatment with nifedipine is strongly advocated. (20 mg slow-release nifedipine every six hours until persistent relief of symptoms).[14] Diuretics are not part of standard protocols because many patients are volume depleted.
In the area where medical infrastructure and assistance is available, vasodilator treatment is not strictly necessary because with bed-rest and supplemental oxygen for 24 to 48 hours, relief of symptoms is achieved within hours and complete clinical recovery should be the standard within several days while staying at the same altitude.[6]
Conclusion
Nowadays, sojourns to high altitude are becoming more frequent for adventure or recreational purpose. Notwithstanding, too rapid ascend or poor adaptability to elevation leads to altitude disorders (AMS), or even lung or cerebral edema if the episode progresses.
Indeed, rapid changes from low altitude to high altitude may cause fatigue, headache, light-headedness and nausea to, at least, one in four people who travel above 3500 meters (11600 feet) and to more than half of those who ascend above 6000 meters (19700 feet). But mild symptoms of AMS might start sooner around 2400 meters or even below.[7]
In a few words, high altitude stress primarily is due to hypoxia of low atmospheric pressure, but dry air, high winds, intense solar radiation (dehydration), extreme cold and exercise (they both elevate oxygen demands) may contribute to AMS. Slow ascents, gradual changes, increasing water ingestion and avoiding alcohol and heavy meals are the best tips for travelers. Further advice and supplemental drugs may be needed to support baseline patients and other specific cases at very high altitudes.
Conflict of interest
None
Acknowledgments
None
References
1. Paz A, Steinfeld I, Potasman I. Are we doing our best to educate travelers about the risk of Acute Mountain Sickness? An on-site prospective study in the Himalayas. J Travel Med 2007;14:168-172. doi.org/10.1111/j.1708-8305.2007.00119.X
2. Gaillard S, Dellasanta P, Loutan L, Kaper B. Awareness prevalence, medication use, and risk factors of acute mountain sickness in tourists trekking around the Annapurnas in Nepal: a 12-year follow-up. High Alt Med Biol 2004;5:410-419.
3. Honigman B, Theis MK, Koziol- McLain J, Roach R, Yip R; Houston C. Acute mountain sickness in a general tourist population at moderate altitudes. Ann Intern Med 1993;118:587-592.
4. Theis MK, Honigman B, Yip R, McBride D, Houston CS, Moore LG. Acute mountain sickness in children at 2835 meters. Am J Dis Child 1993;147:143-145.
5. Hornbein TF,TownesBD, Schoene RB, Sutton JR, Houston CS. The cost to the central nervous system of climbing to extremely high altitude. N England J Med 1989;321(25):1714-9. doi:10.1056/NEJM198912213212505
6. West JB. The physiologic basis of high-altitude diseases. AnnIntern med. 2004; 141(10):789-800. Doi: 10.7326/00003-4819-141-10-200411160-00010
7.Meier D, Collet T, Locatelli I, Cornuz J, Kayser B, Simel D,et al. Does this patient have acute Mountain Sickness? the Rational Clinical Examination systematic review. JAMA. 2017;318(18):1810-1819. doi:10.1001/jama.2017.16192.
8. Jin J Acute Mountain Sickness. JAMA. 2017;318(18):1840. doi:10.1001/jama.2017.16077.
9. Hurtado A, Fuquay R, Sirota J, Swenson E, Schoene R, Jefferson et al. High altitude Renal Syndrome (HARS). J Am Soc Nephrol. 2011;22(11):1963-1968. doi:10.1681/ASN.2010121316.
10. Cremona G, Asnaghi R, Baderna P, Brunetto A, Brutsaert T, Cavallaro C et al. Pulmonary extravascular fluid accumulation in recreational climbers: a prospective study. Lancet. 2002;359(9303):303-9. http://dx.doi.org/10.1016/s0140-6736(02)07496-2.
11. Pasha MA, Newman JH. High altitude disorders: pulmonary hypertension: pulmonary disease: the global perspective. Chest.2010;137(6 Suppl):13S-19S. doi: 10.1378/chest.09-2445.
12. Swapnil, J Paralikar. High altitude pulmonary edema clinical features, pathophysiology, prevention and treatment. Indian J Occup Environ Med. 2012; 16(2):59–62. doi: 10.4103/0019-5278.107066.
13. Penaloza D, Arias-Stella J. The heart and pulmonary circulation at high altitudes. Circulation. 2007;115:1132-1146. https://doi.org/10.1161/CIRCULATIONha.106.624544
14. Bartsch P, Maggiorini M, Ritter M, Noti C, Vock P, Oelz O. Prevention of high- altitude pulmonary edema by nifedipine. N England J Med.1991;325(18):1284-1289.
15. Deshwal R, Iqbal M, Basnet S. Nifedipine for the treatment of high altitude pulmonary edema. Wilderness Environ Med. 2012;23(1):7-10. doi:10.1016/j.wem.2011.10.003.
16. Sartori C, Allemann Y, Duplain H, Lepori M, Egli M, Lippe, et al. Salmeterol for the prevention of high-altitude pulmonary edema. N Engl J Med. 2002;346; 1631-6.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/