J Med Discov (2017); 2(4):jmd17047; DOI:10.24262/jmd.2.4.17047; Received September 25th, 2017, Revised October 18th, 2017, Accepted October 20th, 2017, Published October 22nd, 2017.
A clinical analysis of retropharyngeal lymph node metastasis from oral tongue carcinoma
Liu Tian-Run1,#, Wang Wei1,#, Zhuang Shi-Min1,#, Xie Liang-En1, Zhang Guan-Ping1, Long Zhen1, Wei Fan-Qin1, Xiao Zhi-Wen1, Sun Xiao-Mei1, Yang An-Kui2,3,*
1. Department of Otorhinolaryngology Head and Neck Surgery, The Sixth Affiliated Hospital of Sun Yat-sen University, Guangzhou, China, 510655.
2. Department of Head and Neck Surgery, Sun Yat-sen University Cancer Center, Guangzhou, China, 510060.
3. State Key Laboratory of Southern China, Guangzhou, China, 510060.
* Correspondence: Ankui Yang, Department of Head and Neck Surgery, Sun Yat-sen University Cancer Center, Guangzhou, China, 510060. yangak@sysucc.org.cn
# Contributed equally.
Abstract
Background: Lymph node metastasis occurs commonly in level I to level III area of neck in patients with oral tongue carcinoma. The incidence of retropharyngeal lymph node metastasis (RPLNM) from oral tongue carcinoma is very rare. However, in some postoperative cases, RPLNM possibly occurs in retropharyngeal region.
Objective: In this study, we investigated clinical features, treatment and prognosis of oral tongue carcinoma patients with RPLNM.
Methods: The data of 6 subjects with RPLNM from oral tongue carcinoma treated from April 2000 to April 2005 were retrospectively analyzed. The incidence, clinical manifestation, imaging characteristics, treatment, and prognosis were reviewed and described.
Results: Among the 176 treated patients with established diagnose of oral tongue squamous cell carcinoma, 6 underwent recurrence in retropharyngeal lymph node, and the incidence was 3.41% (6/176). All the 6 patients had underwent neck dissection before the occurrence of RPLNM; the recurrence interval was 5 to 19 months with a median time of 9 months. Three patients were treated with radiotherapy including the other 3 with chemotherapy. The survival time of all patients ranged from 3 to 45 months with the medial time of 17.2 months.
Conclusions: RPLNM from oral tongue carcinoma indicates malignant behavior with extremely poor prognosis. Radiotherapy might be a way to improve overall survival.
Keywords: Oral neoplasms; retropharyngeal lymph node metastasis; prognosis.
Introduction
The incidence of retropharyngeal lymph node metastasis (RPLNM) in patients with oral tongue cancer is very low, and the retropharyngeal space is a potential space located between the posterior pharyngeal wall and prevertebral fascia [1-3]. For these reasons, RPLNM is easily to be omitted [2, 3]. This study aimed to analyze the metastasis pattern, diagnosis and treatment of RPLNM by retrospective study of the relevant oral tongue carcinoma cases.
Subjects and Methods
Clinical data
The patient group included 4 males and 2 females, and the age ranged from 41 to 64 years, with the median age of 49 years old. The common features included: (1) the primary tumor located in the oral tongue with confirmed pathological diagnosis of squamous cell carcinoma; (2) all the patients had neck dissection surgery history before the occurrence of RPLNM. All relapsed occurred in retropharyngeal lymph node with no recurrence in primary site; (3) operation procedures included ipsilateral neck lymph node dissection; (4) the clinical manifestations and imaging characteristics were similar during relapsing.
According to TNM staging of UICC/IJCC in 2010, the primary postoperative pathological stages were: T1 in 1 case, T2 in 2 cases and T3 in 3 cases; N0 in 1 case, N1 on 2 cases and N2 in 3 cases. None of the patients had distant metastasis.
All the patients received hemiglossectomy with ipsilateral level I to III neck dissection. Six patients relapsed in unilateral retropharyngeal lymph node in the following 6 to 9 months after surgery, including 5 cases in ipsilateral retropharyngeal lymph node, and 1 in the contralateral side. Four cases had ipsilateral cervical level II area lymph node metastasis simultaneously with RPLNM. Then these 6 patients underwent radical neck dissection.
Treatment
Three of the 6 cases associated with RPLNM received radical treatment such as radiotherapy, while the rest 3 cases had palliative chemotherapy. Chemotherapy regimen was DBF: Cisplatin, 30 mg/m2, day 1-3; Fluorouracil, 600 mg/m2, day 1-5; Bleomycin, 8 mg/m2, day1, day3 and day5.
Follow-up time and methods
Follow-up information was obtained by telephone contacts and outpatient visits. The follow-up time started from the date of diagnosis and ended in October 2007.
Results
The occurrence of retropharyngeal lymph node metastasis from oral tongue carcinoma
From April 2000 to April 2005, 176 patients in our hospital were diagnosed as oral tongue squamous cell carcinoma and received surgical treatments. All the cases were followed up and 6 of them had retropharyngeal lymph node metastasis. The incidence of RPLNM was 3.41% (6/176). The time interval of recurrence of retropharyngeal lymph node metastasis after last neck dissection was 5 to 19 months with the median time of 9 months.
Clinical manifestations and imaging characteristics
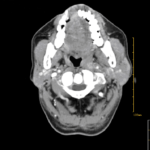
Clinical manifestations and imaging characteristics after relapsing were similar among these patients. Five cases had pain and swelling in posterior region of mandible, one of them also accompanied by hoarseness and sore throat; one case had oropharyngeal mass with sore throat. All the imaging (CT) results showed soft tissue appearance with uneven density or central necrosis in the left retropharyngeal space, and the shortest diameters were more than 10 mm. The feature of the pictures was in line with malignant tumor cervical lymph node metastasis imaging diagnostic criteria (Figure 1). In one case, we obtained pathologic evidence by biopsy.
Figure 1. CT shows retropharyngeal lymph node metastasis
Results of follow-up
Until the last follow-up in October 2007, there were 2 cases of survival while 4 cases dead from tumor-related diseases. No patient was lost in follow-up. The average follow-up was 41 months, with a varied follow-up period of 32 to 59 months.
Treatment and overall survival
Three patients received radical radiotherapy and the treatment results were as follows. (1) One patient had concurrent chemoradiotherapy (70 Gy). Retropharyngeal lesion disappeared after radical radiotherapy/ chemoradiotherapy, and there was no recurrence of retropharyngeal metastasis during the next 45 months after treatment. (2) Another patient found lung metastasis when the dose of radiotherapy reached 39 Gy, then he received palliative chemotherapy instead of DBF regimen. This patient died of cancer-related diseases 9 months later. (3) The last case had residual tumor after radio treatment, but has survived with tumor in the next 31 months.
Three patients were treated by palliative chemotherapy, however, the effect was not significant. Patients survived 3 to 9 months with tumor respectively.
Up to October 2007, the cancer-specific survival time of the six patients ranged from3 to 45 months with the mean time of 17.2 months.
Discussion
The incidence and pathogenesis of retropharyngeal lymph node metastasis
The retropharyngeal space is a potential space located between the posterior pharyngeal wall and the prevertebral layer fascia, more medially than internal carotid sheath [2, 4]. The uppermost part goes to skull base and the lower part down to the level of T4. It is generally believed that lymphatic metastasis of tumor cells have two patterns: anterograde metastasis and retrograde metastasis [5]. Besides those, some people bring out lymphatic spread theory [5-7]. Regardless, all these theories come to the same result that tumor cells accumulate in lymph nodes, forming new tumor lesions in appropriate conditions [5-7].
The location cervical lymph node metastasis of oral tongue carcinoma is closely associated with the location of primary lesion. Generally, tongue cancer cells spread to the upper deep cervical, submandibular, and omohyoid lymph nodes due to anterograde metastasis [8-11]. But tongue cancer can also present irregular lymph node metastasis, such as retrograde metastasis which is often seen in recurrent cases. The possible reason for retrograde metastasis is that tumor embolization or surgery (such as neck dissection) changed lymphatic drainage pathways, and enabled the tumor cells to be transferred in a quite different way. According to the anatomical features of tongue cancer cells’ lymphatic drainage pathway and the retrograde metastasis theory, we may consider the retropharyngeal lymph node metastasis of tongue cancer as another manifestation of its retrograde metastasis [3]. Mechanisms could be the following two hypothesis: (1) After arriving at upper deep cervical lymph node area (level II), tumor cells form an embolization, which blocks the pathway of lymphatic drainage and contributes to the retrograde metastasis to retropharyngeal lymph nodes; (2) neck dissection changes the lymphatic drainage pathway in the neck postoperatively. Tumor cells metastasize to retropharyngeal lymph node without passing the area of level II. RPLNM developed in this way always has primary tumor lesions in the beginning of recurrence. Neck dissection often leads to a series of changes in normal lymphatic drainage pathways; for instance, a significant reduction in the number or density of lymphatic ducts in the surgical area may lead to a compensatory increase in lymphatic channels outside the surgical area. Tumor cells originated from the primary lesions or regional lymph nodes can be directly transferred to the retropharyngeal lymph nodes by these side pathways [5, 7]. In this group, all the 6 patients had upper deep cervical (level II) lymph node metastasis before the RPLNM [12].
Clinical manifestations and imaging characteristics
Patients with RPLNM had similar clinical manifestations and imaging characteristics. The main manifestations of the six patients were pain and swelling in posterior region of mandible. Hoarseness and sore throat occurred in 1 case as well. Imaging (CT mainly) studies of all the patients showed soft-tissue neoplasm appearance in the retropharyngeal space. The diameter of the lymph node was greater than 10 mm, with uneven density or central necrosis. The features of the lymph nodes were in accordance with the imaging diagnostic criteria of malignant lymph node metastasis.
It is still controversial of the RPLNM imaging diagnostic criteria. Mancuso and associates [5] believed that the sizes of retropharyngeal metastatic lymph nodes were between 7 -30 mm with a general size more than 10 mm, and the imaging of lymph nodes always presented rim enhancement or necrotic core in the picture. So they set the diameter of 10 mm as the cutoff, which we had applied in this study; also, Watarai used 8 mm as the standard [13]. According to David et al, the diagnosis RPLNM only by CT image has an accuracy of 70% [14], which means we need more examination methods to confirm the diagnosis. However, it is hard to get pathologic evidence by biopsy or other options. One of the six cases in this group had pathologic evidence by biopsy. Therefore, we believed that oral tongue carcinoma patients, especially postoperative cases who have manifestations, such as pain or swelling in the posterior mandibular area, sore throat, hoarseness, Horner’s syndrome and jugular foramen syndrome, should be alert to RPLNM. We advise such patients to have imaging examination (such as CT, MRI, PET-CT), pathology and other related tests to confirm the diagnosis.
Therapeutic strategy decision and evaluation
Some scholars suggested that patients with RPLNM should be given radical or adjuvant radiotherapy [1, 2, 15]. Spencer, C. R. and associates recommend doses of 70 Gy, while we recommend the dose of 66 Gy [15]. In our group of patients, two cases had radical radiotherapy in retropharyngeal lymph node area, one of them had complete response (CR), and still survived without tumor till the last follow-up. David et al. suggested surgical treatment to patients with RPLNM [14]. Primary site surgery and radical neck dissection can be performed concurrently or separately. Tseng, JR’s study also showed surgical treatment improved survival of patients with oral cavity cancer [6]. Therefore, further studies are needed to evaluate the difference of the treatment effect between radiotherapy and surgery. Oral tongue carcinoma patients with RPLNM always have poor prognosis [6, 13], likewise, the medial survival time of all the 6 patients was 17.2 months with the range from 3 to 45 months.
In conclusion, oral tongue carcinoma patients with RPLNM always have extremely poor prognosis [6,13]. There are only few studies focusing on this kind of disease. We need more evidence about the efficacy of surgery and radiotherapy, in order to compare the two options. Furthermore, the best treatment strategy remains to be defined.
Acknowledgments
This work was supported by National Natural Science Foundation of China (No. 81272955 and 81302368) and Guangdong Province Natural Science Foundation (2015A030313058).
References
- Gross ND, Ellingson TW, Wax MK, Cohen JI, Andersen PE. Impact of retropharyngeal lymph node metastasis in head and neck squamous cell carcinoma. Arch Otolaryngol Head Neck Surg. 2004;130(2):169-73. doi: 10.1001/archotol.130.2.169. PubMed PMID: 14967745.
- Layland MK, Sessions DG, Lenox J. The influence of lymph node metastasis in the treatment of squamous cell carcinoma of the oral cavity, oropharynx, larynx, and hypopharynx: N0 versus N+. Laryngoscope. 2005;115(4):629-39. doi: 10.1097/01.mlg.0000161338.54515.b1. PubMed PMID: 15805872.
- Nishida M, Yasuda S, Murakami K, Yamamura I, Nagata Y, Iizuka T. Retropharyngeal lymph node metastases from oral cancer: a report of 2 patients. J Oral Maxillofac Surg. 2005;63(3):410-2. doi: 10.1016/j.joms.2004.04.035. PubMed PMID: 15742298.
- Umeda M, Shigeta T, Takahashi H, Kataoka T, Oguni A, Minamikawa T, et al. Metastasis to the lateral retropharyngeal lymph node from squamous cell carcinoma of the oral cavity: report of three cases. Int J Oral Maxillofac Surg. 2009;38(9):1004-8. doi: 10.1016/j.ijom.2009.04.015. PubMed PMID: 19467843.
- Chen LL, Blumm N, Christakis NA, Barabasi AL, Deisboeck TS. Cancer metastasis networks and the prediction of progression patterns. Br J Cancer. 2009;101(5):749-58. doi: 10.1038/sj.bjc.6605214. PubMed PMID: 19707203; PubMed Central PMCID: PMCPMC2736851.
- Tseng JR, Ho TY, Lin CY, Lee LY, Wang HM, Liao CT, et al. Clinical outcomes of patients with oral cavity squamous cell carcinoma and retropharyngeal lymph node metastasis identified by FDG PET/CT. PLoS One. 2013;8(11):e79766. doi: 10.1371/journal.pone.0079766. PubMed PMID: 24244559; PubMed Central PMCID: PMCPMC3823565.
- Cady B. Regional lymph node metastases; a singular manifestation of the process of clinical metastases in cancer: contemporary animal research and clinical reports suggest unifying concepts. Ann Surg Oncol. 2007;14(6):1790-800. doi: 10.1245/s10434-006-9234-2. PubMed PMID: 17342568.
- Abu-Ghanem S, Yehuda M, Carmel NN, Leshno M, Abergel A, Gutfeld O, et al. Elective Neck Dissection vs Observation in Early-Stage Squamous Cell Carcinoma of the Oral Tongue With No Clinically Apparent Lymph Node Metastasis in the Neck: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg. 2016;142(9):857-65. doi: 10.1001/jamaoto.2016.1281. PubMed PMID: 27442962.
- Jarungroongruangchai W, Charoenpitakchai M, Silpeeyodom T, Pruksapong C, Burusapat C. Size of cervical lymph node and metastasis in squamous cell carcinoma of the oral tongue and floor of mouth. J Med Assoc Thai. 2014;97 Suppl 2:S101-6. PubMed PMID: 25518182.
- Sano D, Myers JN. Metastasis of squamous cell carcinoma of the oral tongue. Cancer Metastasis Rev. 2007;26(3-4):645-62. doi: 10.1007/s10555-007-9082-y. PubMed PMID: 17768600.
- Yang AK, Liu TR, Chen FJ, Ma XF, Guo ZM, Song M, et al. [Survival analysis of 229 patients with advanced squamous cell carcinoma of the oral tongue]. Ai Zheng. 2008;27(12):1315-20. PubMed PMID: 19080001.
- Van Trappen PO, Pepper MS. Lymphatic dissemination of tumour cells and the formation of micrometastases. Lancet Oncol. 2002;3(1):44-52. PubMed PMID: 11905605.
- Watarai J, Seino Y, Kobayashi M, Shindo M, Kato T. CT of retropharyngeal lymph node metastasis from maxillary carcinoma. Acta Radiol. 1993;34(5):492-5. PubMed PMID: 8396404.
- Morrissey DD, Talbot JM, Cohen JI, Wax MK, Andersen PE. Accuracy of computed tomography in determining the presence or absence of metastatic retropharyngeal adenopathy. Arch Otolaryngol Head Neck Surg. 2000;126(12):1478-81. PubMed PMID: 11115286.
- Spencer CR, Gay HA, Haughey BH, Nussenbaum B, Adkins DR, Wildes TM, et al. Eliminating radiotherapy to the contralateral retropharyngeal and high level II lymph nodes in head and neck squamous cell carcinoma is safe and improves quality of life. Cancer. 2014;120(24):3994-4002. doi: 10.1002/cncr.28938. PubMed PMID: 25143048; PubMed Central PMCID: PMCPMC4257883.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/