J Med Discov (2017); 2(2):jmd17016; DOI:10.24262/jmd.2.2.17016; Received April 20th, 2017, Revised May 17th, 2017, Accepted May 17th, 2017, Published May 26th, 2017.
Complete Disappearance of Barrett’s Epithelial Metaplasia Following Long Term Proton Pump Inhibitor Therapy
Baher AL-Abbasi1, Ayat AL-Rubaye1, Nisar Ahmed1
1 Department of Gastroenterology, Park Plaza Hospital, Houston, TX 77004 USA
* Correspondence: Dr. Nisar Ahmed, M.D. , F.A.C.G. Chief of Gastroenterology, Park Plaza Hospital, Houston, TX 77004, USA. Email:nisarahmedmd@yahoo.com.
Abstract
The previous paradigm that Barrett’s epithelial metaplasia is an irreversible premalignant condition has recently been challenged by evolution of reports and studies that documents partial or complete regression of Barrett’s metaplasia by long term medical therapy with endoscopic and histological follow up . This case documents complete regression of intestinal metaplasia in esophagus after long term proton pump inhibitor therapy with endoscopic and histological follow up.
Keywords: Barrett’s esophagus, Proton pump inhibitor, Endoscopy, chronic gastro-esophageal reflux disease.
Introduction
Barrett’s esophagus is thought to be a premalignant condition secondary to chronic gastro-esophageal reflux disease[1].It is an abnormal change (metaplasia) in the cells of the lower portion of the esophagus,characterized by the replacement of the normal stratified squamous epithelium lining of the esophagus by specialized intestinal epithelium with goblet cells.The medical significance of Barrett’s esophagus is its strong association (about 0.5% per patient-year) with esophageal adenocarcinoma,a very often deadly cancer,[2][3]because of that it is considered to be a premalignant condition.We describe a case of Barrett’s epithelial metaplasia that completely eliminated after several years of treatment with proton pump inhibitor.
Case Report
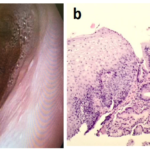
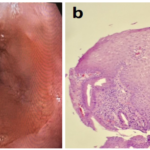
A 67 years old Caucasian gentleman underwent Esophagogastroduodenoscopy (EGD) for evaluation of longstanding heartburn for which he had used over the counter medicines only with partial relief. EGD showed evidence of early Barrett’s esophagus (Fig.1a). Biopsy also confirmed presence of specialized intestinal metaplasia (Fig. 1b). Patient was put on pantoprazole 40 mg daily AM. Pantoprazole is a proton pump inhibitor for the treatment of erosive esophagitis and other conditions involving high level of stomach acid. Four years later he has another EGD which showed mild gastroesophageal reflux disease (GERD) but no salmon colored mucosal islands (Fig.2a).Biopsies taken showed no Barrett’s metaplasia (Fig.2b). One year later EGD was done and despite it showed mild GERD with pink colored mucosa (Fig.3a), but the biopsies again showed no evidence of Barrett’s metaplasia (Fig.3b). Patient took pantoprazole up to the last EGD but after that was switched to famotidine 20 mg at bedtime, he has remained symptom free.
Figure 1. Early Barrett’s esophagus. Endoscopic view (a) shows early Barrett’s esophagus with salmon colored mucosal islands. Microscopic view (b) shows specialized intestinal metaplasia.
Figure 2. Mild GERD. Endoscopic view (a) shows mild GERD without salmon colored mucosal islands. Microscopic view (b) shows normal squamocolumnar junction with absence of goblet cells.
Figure 3. Mild GERD . Endoscopic view (a) shows mild GERD with pink colored mucosa. Microscopic view (b) shows squamocolumnar junction with absence of goblets cells.
Discussion
Barrett’s esophagus is a condition in which squamous epithelium of the esophagus has been replaced by specialized intestinal epithelium with goblet cells.Barret’s esophagus is a premalignant condition;with 10 fold increased risk for esophageal cancer compared to the risk in general population[4].Currently the treatment of Barrett’s esophagus is aimed at several targets which include symptom relief,healing of esophagitis and prevention of peptic stenosis;these objectives are nowadays well achieved by medical acid suppression therapy using either H2 blocker or preferentially proton pump inhibitor and by antireflux surgery,all these modalities accompanied by life style changes.The risk of esophageal adenocarcinoma in Barrett’s patient correlates with the severity of GERD,the length of the Barrett’s segment and the presence of dysplasia[5][6].This cancer risk might therefore be decreased by complete reversion of the metaplasia into normal squamous epithelium.Barrett’s metaplasia results from chronic exposure of distal esophagus to gastric acid.This reflux has been reduced by proton pump inhibitor therapy and other antireflux measures which may lead to Barrett’s regression as seen in this case and other numerous studies[7][8][9][10],in contrary to the known idea that Barrett’s esophagus is an irreversible condition. However the optimal form of antireflux therapy to affect reversal of Barrett’s esophagus is as yet unknown.
Conclusion
As Barrett’s esophagus result from chronic GERD, Barrett regression can theoretically be obtained by antireflux treatment,thus a decrease of cancer risk might be anticipated if treatment could induce a regression of Barrett’s epithelial metaplasia. This case report adds to the growing body of literature suggesting Barrett’s esophagus can be totally eliminated, with long term proton pump inhibitor therapy with endoscopic and histological follow up,in this case the elimination of Barrett’s metaplasia may be due to optimum antireflux treatment used or/and due to small island of metaplasia that was removed by multiple biopsies .
Conflict of interest
No conflict of interest to disclose, we have received no support or commercial funding for this case report,or for any products mentioned herein.
Acknowledgment
We would like to express our appreciation to Dr. Robyn A. Beach M.D. for his valuable help.
References
1. Fennerty MB. Barrett’s esophagus: What do we really Know about this disease? Am J Gastroenterol 1997;92(1):1-3. PMID:8995929.
2. Shaheen NJ, Richter JE (March 2009). “Barrettoesophagus”. Lancet. 373 (9666):850-61.DOI:10.1016/S0140.6736(09)60487.6. PMID 19269522.
3. Koppert LB, Wijnhoven BP, van Dekken H, Tilanus HW, DinjensWN (2005). “The molecular biology of esophageal adenocarcinoma”. J Surg Oncol. 92 (3):169.90. doi:10.1002/jso.20359. PMID 16299787.
4. Polednak AP (May 2003). “Trends in survival for both histologic types of esophageal cancer in US surveillance, epidemiology and end results areas”. Int.J.Cancer. 105 (1):98.100. doi:10.1002/ijc.11029. PMID 12672037.
5. Iftikhar SY,James PD, Steele RJG, et al.Lenghth of Barrett’s oesophagus: an important factor in the development of dysplasia and adenocarcinoma. Gut 1992;33:1155-8 . PMID:1427364 .
6. Menke Pluymers MBE, Hop WCJ, Dees J, et al. Risk factors for the development of an adenocarcinoma in columnar-lined(Barrett) esophagus. Cancer 1993;72:1155-8 . PMID:8339208
7. Peters FT1, Ganesh S, Kuipers EJ, Sluiter WJ, Klinkenberg-Knol EC, Lamers CB, https://www.ncbi.nlm.nih.gov/pubmed/term=Kleibeuker%20JH%5BAuthor%5D&cauthor=true&cauthor_uid=10486353et al.
Endoscopic regression of Barrett’s oesophagus during omeprazole treatment;a randomised double blind study. Gut. 1999 Oct;45(4):489-94. PMID:10486353.
8. Malesci A1, Savarino V, Zentilin P, Belicchi M, Mela GS, Lapertosa G, et al. Partial regression of Barrett’s esophagus by long-term therapy with high-dose omeprazole. Gastrointest Endosc. 1996 Dec;44(6):700-5. PMID: 8979061.
9. Horwhat JD1, Baroni D, Maydonovitch C, Osgard E, Ormseth E, Rueda-Pedraza E, et al. Normalization of intestinal metaplasia in the esophagus and esophagogastric junction: incidence and clinical data.Am J Gastroenterol. 2007 Mar;102(3):497-506.PMID: 17156135. DOI: 10.1111/j.1572.0241.2006.00994.x
10. Weston AP1, Krmpotich PT, Cherian R, Dixon A, Topalosvki M. Prospective long-term endoscopic and histological follow-up of short segment Barrett’s esophagus: comparison with traditional long segment Barrett’s esophagus. Am J Gastroenterol. 1997 Mar;92(3):407-13. PMID:9068459.
11. Ottenjann R, Heidt H. Regression der Zyllinderepithel-metaplasie bei barrett-Oesophagus.Dtsch Med Wochenschr 1990;115(23):916-17. PMID: 2354665
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/