Journal of Medical Discovery (2017); 2(1):jmd16009; doi:10.24262/jmd.2.1.16009; Received November 7th,2016, Revised November 21st,2016, Accepted November 21st, 2016, Published February 10st,2017.
PR1 Peptide Vaccine For Myeloid Leukemia
Zubair Shahid Bashir1,*, Muzaffar H. Qazilbash1
1Department of Stem Cell Transplantation and Cellular Therapy, University of Texas MD Anderson Cancer Center, houston, TX,77030
* Correspondence: Dr. Zubair Shahid Bashir, 2386-B Birch Run Circle, Herndon, VA, 20171. Email: shahid.zubair08@gmail.com. Tel: +1-708-340-2832
Pictorial Summary
Figure 1. Structure and function of proteinase 3.
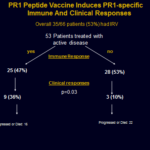
Figure 2. PR1 peptide vaccine induces PR1-specific immune and clinical response.
Commentary
PR1 is an HLA-A2-restricted peptide derived from both proteinase 3 and neutrophil elastase in myeloid leukemia cells. It is recognized as leukemia antigen by cytotoxic T lymphocytes (CTLs) that preferentially kill leukemia and contribute to clinical remission (1-2). In this trial, the authors evaluated the safety, immunogenicity and clinical activity of PR1 peptide as a vaccine in 66 HLA-A2+ patients with acute myeloid leukemia (AML: 42), chronic myeloid leukemia (CML: 13) or myelodysplastic syndrome (MDS: 11). These patients received three to six PR1 peptide vaccinations, administered subcutaneously every 3 weeks at one of three dose levels. Authors report that PR1-specific CTL (PR1-CTL) immune responses were noted in 35 of 66 (53%) patients. In the 53 evaluable patients with active disease, 12 (24%) patients had objective clinical responses. Interestingly, clinical responses were predominantly seen in patients who demonstrated a PR1-specific immune response. The authors conclude that PR1 peptide vaccine induces peptide-specific immunity that correlates with clinical responses, including molecular remission, in patients with AML, CML and MDS.
There has been a great interest in harnessing the power of patient’s own immune system against their cancer. Although this approach is based on sound scientific rationale, the overall progress has been slow until the last few years. That is now rapidly changing with recent exciting results by using immunotherapy approaches like vaccines, monoclonal antibodies, immune checkpoint inhibitors and engineered T cells targeting cancer proteins (CAR-T cells). An example of this is the generation of immune specific T cells derived from BCR-ABL fusion region within 9;22 translocation in CML shown previously (3-5). However, our trial adds to a growing list of immune-based therapies. It is well known that cytotoxic T lymphocytes (CTL) are perhaps the strongest mediators of anti-tumor immunity and have the ability to keep the proliferating cancer cells in check. The CTLs work by recognizing and targeting cancer antigens that are presented by malignant cells in combination with major histocompatibility (MHC) molecules (1). In this trial, the investigators used PR1 peptide antigen as a vaccine. Because immunotherapy can flare up underlying autoimmune diseases, the investigators excluded patients with known autoimmune diseases, specifically Wegener’s granulomatosis, where anti-proteinase 3 antibodies may exacerbate the underlying disease.
The primary purpose of the study was to determine the safety of the vaccine, and to determine if the vaccine could induce anti-leukemia immune response. This large vaccine trial clearly showed the safety of this vaccine, with minor injection site erythema being the most common adverse event. Importantly, there was no flare up of vasculitis. Furthermore, there was no worsening of Graft Versus Host Disease, cytopenias, or the emergence of c-ANCA, an antibody associated with Wegener’s granulomatosis. The immune response, determined by the doubling of PR1-CTL compared to baseline, was observed in 53% of the treated patients (6). In 53 patients with active disease at enrollment, 24% had clinical responses defined as complete remission, partial remission or hematologic improvement (7). Authors showed that generation of PR1-CTL was independent of pre-existing PR1-CTLs in the peripheral blood but was influenced by disease burden and the age of the patient. Younger age was associated with more robust immune response which might be related to the thymic function. As expected in immune-based approaches, a high tumor burden overwhelms the slowly developing anti-tumor immune response. It can be argued that as the disease burden increases, the effectiveness of PR1-CTL decreases. This is due to selective elimination of high-avidity PR1-CTL (8). Authors also reported the durability of immunologic and clinical response in selected patients. They showed that vaccine-specific T cells were highly enriched in central memory phenotype, which might have conferred a long-term anti-leukemia immunity.
The clinical responses were seen in all 3 myeloid leukemia groups, predominantly in patients with low disease burden. There was a strong correlation between vaccine-specific immune response and achievement of clinical response in this trial. One of the strengths of this trial is the long-term follow up, with a median follow up duration of 10 years. The 10-year overall survival was 38% and 10-year event free survival was 20% which were both longer in patients with immune responses and clinical responses. The authors conclude that this vaccine can potentially be used in patients with low disease burden, or those who are in remission but at a higher risk of relapse. They also propose that combining it with checkpoint inhibitors may further enhance the effectiveness of this vaccine.
Competing interests
The authors declare that they have no competing interests.
Acknowledgments
This work was supported by grants from NIH (CA81247, CA49639, CA100632) and supported by Leukemia and Lymphoma Society.
References
1. Molldrem JJ. Vaccination for leukemia. Biol Blood Marrow Transplant 2006 Jan; 12(1 Suppl 1): 13-18.
2. Molldrem J, Dermime S, Parker K, Jiang YZ, Mavroudis D, Hensel N, et al. Targeted T-cell therapy for human leukemia: cytotoxic T lymphocytes specific for a peptide derived from proteinase 3 preferentially lyse human myeloid leukemia cells. Blood 1996 Oct 1; 88(7): 2450-2457.
3. Cathcart K, Pinilla-Ibarz J, Korontsvit T, Schwartz J, Zakhaleva V, Papadopoulos EB, et al. A multivalent bcr-abl fusion peptide vaccination trial in patients with chronic myloid leukemia. Blood 2004 Feb 1; 103(3): 1037-1042.
4. Bocchia M, Gentili S, Abruzzese E, Fanelli A, Iuliano F, Tabilio A, et al. Effect of a p210 multipeptide vaccine associated with imatinib or interferon in patients with chronic myeloid leukaemia and persistent residual disease: a multicentre observational trial. Lancet 2005 Feb 19-25; 365(9460): 657-662.
5. Maslak PG, Dao T, Gomez M, Chanel S, Packin J, Korontsvit T, et al. A pilot vaccination trial of synthetic analog peptides derived from the BCR-ABL breakpoints in CML patients with minimal disease. Leukemia 2008 Aug; 22(8):1613-1616.
6. Molldrem JJ, Clave E, Jiang YZ, Mavroudis D, Raptis A, Hensel N, et al. Cytotoxic T lymphocytes specific for a nonpolymorphic proteinase 3 peptide preferentially inhibit chronic myeloid leukemia colony-forming units. Blood 1997 Oct 1; 90(7): 2529-2534.
7. Cheson BD, Bennett JM, Kantarjian H, Pinto A, Schiffer CA, Nimer SD, et al. Report of an international working group to standardize response criteria for myelodysplastic syndromes. Blood 2000 Dec 1; 96(12): 3671-3674.
8. Molldrem JJ, Lee PP, Kant S, Wieder E, Jiang W, Lu S, et al. Chronic myelogenous leukemia shapes host immunity by selective deletion of high-avidity leukemia-specific T cells. The Journal of clinical investigation 2003 Mar; 111(5):639-647.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/