J Med Discov (2020); 5(4):jmd20060; DOI:10.24262/jmd.5.4.20060; Received August 05th, 2020, Revised September 28th, 2020, Accepted October 25th, 2020, Published November 3rd,2020.
Capnography As A Predictive Value In Cardiopulmonary Resuscitation: A Systematic Review
Eva Codina-Diaz1, Manuel Piñero-Zapata (PhD)1,2, Amelia Canovas-Miralles2
1 Nursing Faculty, San Antonio Catholic University of Murcia (UCAM), Murcia, Spain.
2 Mobile Emergencies Unit, Gerencia de Urgencias y Emergencias 061, Servicio Murciano de Salud, Murcia, Spain.
* Correspondence:Manuel Piñero-Zapata, Calle Travesía Segunda Parque, 19–Las Torres de Cotillas–30565–Murcia–Spain. E-mail: manuelpinerozapata@gmail.com
Abstract
Background: Cardiac arrest (CA) is considered one of the main public health problems in the world. Knowing how to predict a successful outcome of it early, is one of the main challenges for professionals in the healthcare world. In recent years, capnography has become important in the world of intra and out-of-hospital emergencies, being a great help during resuscitation efforts.
Objectives: To determine if the values of the capnograph during cardiopulmonary resuscitation predict return of spontaneous circulation (ROSC).
Methodology: Systematic review of the available scientific literature was carried out, following previously established inclusion and exclusion criteria.
Results and Conclusions: A total of 6 articles were selected, where it was observed that the capnograph can be used in an acceptable way to predict ROSC. Furthermore, its combination with other parameters can be very useful for decision making. However, there is still no consensus to determine the optimal cut-off point of end-tidal carbon dioxide (EtCO2) to predict ROSC due to the influence of certain confusion factors.
Keywords:capnography, heart attack, end-tidal carbon dioxide, return of spontaneous circulation, cardiac arrest.
Introduction
Cardiorespiratory arrest (CRA) is one of the main causes of death in industrialized countries. Only in Spain there are 18,000 cases of CRA per year in hospitals and 50,000 at the out-of-hospital level, that is why it is considered a public health problem of great importance(1).
The probability of overall survival in Spain after an extra-hospital CRA is 10.1%, slightly lower than the European one (10.7%)(1). These data make it necessary to propose new action strategies in order to improve the results and quality of life of patients who have suffered CA(2). In recent years, the role of capnography has been gaining relevance in the world of intra- and out-of-hospital emergencies, recommending its use during CPR and urgent cardiovascular treatment(3).
Capnographic monitoring consists of the continuous and non-invasive measurement of the carbon dioxide (CO2) exhaled by the patient in the airway(4). The concentration of this degradation product in the body is maximum at the end of expiration, so this parameter, the CO2 at the end of expiration (End-tidal CO2/EtCO2), is the most used to assess the patient’s ventilatory status(5).
The EtCO2 values correlate with the arterial pressure of CO2 (PaCO2) obtained in arterial blood gas. Normal PaCO2 figures are between 35 and 45 mmHg. in healthy patients, EtCO2 figures are 3 to 5 mmHg lower than PaCO2. However, in patients who have an alteration in the Ventilation/Perfusion ratio, these figures may differ by up to 10 mmHg, so they should be kept in mind in clinical practice(6).
In advanced CPR, capnography is used to continuously assess the patient’s hemodynamic status. Some authors point out that during chest compressions the cardiac output is less than 30%, which causes low EtCO2 levels. For a quality cardiac massage, exhaled CO2 values between 15 and 20 mmHg should be achieved. On the other hand, low EtCO2 values during CPR have been associated with a lower probability of ROSC and, therefore, with higher mortality(7,8).
One of the main problems that can occur during advanced CPR is esophageal intubation. Capnography allows to objectively verify the correct placement of the endotracheal tube. Furthermore, it gives us information in real time about possible tube obstructions or accidental extubation(7). Likewise, the European Resuscitation Council (ERC), in its 2015 Resuscitation Guide, recommends the use of capnography to check the correct position of the endotracheal tube in the airway, determine the effectiveness of chest compressions and assess the respiratory rate during CPR in order to avoid hyperventilation of the patient. On the other hand, it suggests the possible use of capnography values to predict, in many cases, the recovery of ROSC and as a prognosis for survival after discharge(5).
In patients who have suffered from an out-of-hospital CPR, knowing how to predict a successful outcome of CPR early is a great challenge for professional advanced life support providers. Despite the research that has been carried out in recent years, clear conclusions have not yet been reached about the conditions that must be present in the patient in order to accurately predict ROSC(9).
Therefore, we plan to carry out a systematic review of the scientific literature in order to determine the information that capnography can provide us on ROSC and its significance in the patient’s prognosis during CPR.
METHODOLOGY
Given the relevance that the use of capnography has been acquiring during advanced CPR and the multiple studies that have been published in recent years, the present systematic review of the available scientific literature has been carried out, in order to determine whether capnography values during cardiopulmonary resuscitation predict recovery of spontaneous circulation.
The literature search took place between January and April 2020, by collecting different documents, both primary and secondary. The databases and digital platforms used were Pubmed-Medline, ScienceDirect, Web of Sciene (WOS) and The Cochrane Library. The Virtual Health Library (VHL) was also consulted, where we used databases such as IBECS, LILACS and Medline.
The keywords used in the search for the available scientific literature were: “capnography”, “infarction”, “carbon dioxide at the end of expiration”, “recovery of spontaneous circulation” and “cardiac arrest”. The first two are indexed in the MeSH (Medical Subjects Headings) Thesauri.
The Boolean operators used for the combination of the different keywords were “AND” and “OR”. In order to limit the search and obtain the most up-to-date information possible, articles published in the last 5 years were included.
During the selection of scientific articles, a series of inclusion criteria were defined:
- Studies with scientific evidence where ETCO2has been measured during CPR and the results were analyzed.
- Studies of patients over 18 years old who have suffered from a CRA and have undergone CPR, with advanced airway management.
- Studies that have been published from 2015 to 2020.
- Studies published in English or Spanish.
Those articles that did not meet the mentioned criteria were excluded in relation to the subject matter, the age of the study subjects or the period or language of publication. Furthermore, those articles that were not original or primary research were not included.
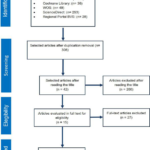
After searching the literature, we made the selection of studies through a careful screening process, reflected by the PRISMA Flow Diagram (Figure 1). First, we eliminated duplicate records and then, through reading the title and full text, we were excluding studies that did not meet the eligibility criteria defined above. The critical reading of the 15 selected articles was carried out using the CASP program (Critical Appraisal Skills Program).
Possible discrepancies in the final selection of these studies were resolved by consensus by two independent reviewers who finally selected 6 articles which are primary investigations (prospective and retrospective studies), that showed sufficient scientific rigor to be kept in mind in the present systematic review.
To establish the levels of scientific evidence and grade of recommendation of the selected articles, the model proposed by the “Scottish Intercollegiate Guidelines Network” (SIGN) was used. This model includes the methodological quality of the studies included in the systematic reviews.
Figure 1. Flow chart for the selection of articles. Source: PRISMA 2009 FlowDiagram. Modified by the author (2020).
RESULTS
The results obtained after analyzing the articles included in this review are presented below.
At the end of this section, a table is shown where the most relevant aspects, level of evidence (LE) and grade of recommendation (GR) for each of them are summarized (Table 1).
Table 1. Summary of articles included in the review of the scientific literature. |
|||||
| Author/Year | LE/GR | Type of Study/n | Objectives | Results | Conclusions |
|
Javaudin M. et al.(10) 2018 |
2++/B |
Retrospective cohort study
n: 9,405 |
Assess the impact, during CPR, of prehospital vital parameters on the neurological result at 30 days. | EtCO2 values <20 mmHg increase the poor neurological prognosis by 19.1%. EtCO2 values <30 or >40 mmHg and SAT >130 or <80 mmHg are indicators of a poor prognosis with AUC 0.87. | EtCO2 values between 30-40 mmHg, SpO2≥94%, and SAT between 100-130 mmHg are associated with a better neurological prognosis. |
|
Engel TW. et al)11) 2019 |
2+/C |
Retrospective cohort study
n: 176 |
Determine the ability of EtCO2 and CerOx to predict ROSC. | EtCO2 was an acceptable predictor of ROSC at different times of CPR with an AUC >0.73, and CerOx an excellent predictor with an AUC >0.81. | Higher values and positive trends in cerebral capnometry and oximetry during resuscitation are associated with greater chances of ROSC. |
|
Poppe M. et al.(12) 2019 |
2++/C |
Retrospective cohort study
n: 526 |
Analyze the value of capnography during CPR to predict ROSC and survival at 30 days. | Baseline EtCO2 values >45 mmHg are associated with a higher probability of punctual ROSC, sustained ROSC and survival at 30 days (p<0.001) when the primary rhythm is Asystolia or PEA. Levels <20 mmHg are associated with a low probability of ROSC (p<0.001). | Patients who have suffered OHCA with an initial non-shockable rhythm and present high initial values of EtCO2, have a greater probability of sustained ROSC and survival at 30 days. |
|
Elola A. et al.(13) 2019 |
2++/B |
Retrospective cohort study
n: 426 |
To determine the capacity of capnography to discriminate between PEA and PR, as well as its potential to detect ROSC. | The joint evaluation of ECG, IT and EtCO2 provide greater discrimination of the PEA/PR segments and, therefore, a greater probability of detecting ROSC with AUC 0.92. EtCO2 levels independently can also be considered an acceptable predictor of ROSC with AUC 0.76. | Capnography offers added value to detect ROSC independently and together with other parameters. |
|
Çalbay A. et al.(14) 2019 |
2++/B |
Retrospective cohort study
n: 155 |
Evaluate whether EtCO2, AaGCO2 and different parameters in blood can be used as a prognostic marker for ROSC. | The PO2, PCO2 and AaGCO2 values were shown to have a statistical significant association with ROSC (p<0.05). EtCO2 levels did not have a significant association with ROSC (p>0.05). | PCO2, PO2, and AaGCO2 values can be used as prognostic markers for ROSC. None of the parameters analyzed were shown to be related to the neurological state of the patient in the short term (p>0.05). |
|
Javaudin F. et al.(15) 2019 |
2+/C |
Multicenter retrospective cohort study
n: 2,239 |
Determine the maximum value of EtCO2 to predict ROSC during CPR in OHCA of traumatic, cardiac and respiratory etiology. | The mean maximum value of EtCO2 during the resuscitation of the subjects was 21.3 mmHg, 28 mmHg and 31.2 mmHg in OHCA of traumatic, cardiac and respiratory causes, respectively. The predictive value of the maximum value of EtCO2 offered an AUC of 0.887, 0.772 and 0.802 for each etiology. | The maximum EtCO2 values were higher in the subjects who achieved ROSC, regardless of the etiology of the OHCA. This measure had a strong diagnostic value for ROSC. |
NOTE: All included studies were conducted on an out-of-hospital cardiac arrest population. Abbreviations: LE: level of evidence; GR: grade of recommendation; n: sample size; CPR: cardiopulmonary resuscitation; EtCO2: end tidal CO2; ROSC: return of spontaneous circulation; PEA: pulseless electrical activity; PR: pulsed rhythms; AaGCO2: arterio-alveolar CO2 gradient; OHCA: out-of-hospital cardiac arrest; AUC: area under curve. |
|||||
Evidence number 1
In 2018, Javaudin et al.(10) investigated the impact of pre-hospital vital parameters on the neurological outcome of patients who have suffered an out-of-hospital cardiac arrest (OHCA).
To do this, they carried out a retrospective cohort study with data extracted from “The French National OHCA Registry”. OHCA produced in adults over 18 years old who were treated by the medical team of advanced life support during the months of July 2011 to July 2017 were included. Patients with traumatic etiology or with a Glasgow scale ≥8 were excluded. Vital parameters that were analyzed were EtCO2, oxygen saturation (SpO2), and systolic blood pressure (SAT).
To assess the neurological deterioration of the patients, the Cerebral Perfomance Categories (CPC) scale was used. The total number of subjects included in the study was 9,405. At the time of hospital discharge after 30 days, 2,382 patients had survived; 1,970 with good neurological status and 412 with poor neurological status.
In the univariate analysis, EtCO2 values were measured in 6,016 subjects (64%), through the endotracheal tube. Both moderate hypocapnia and hypercapnia were found to be associated with a poor prognosis. In fact, the highest probability of a poor neurological outcome occurred with EtCO2 values <20 mmHg, where the risk increased by 19.1% [95% CI (14.3–22.9), p≤0.0001].
A multivariate analysis was also performed in 4,897 subjects, where it was confirmed that EtCO2 values <30 mmHg or >40 mmHg, as well as a TAS >130 mmHg or <80 mmHg, were indicators of poor prognosis. The area under the ROC curve (AUC) of this analysis offered a diagnostic value of 87% [(95% CI (86–88)].
The authors concluded their research by stating that the EtCO2, SpO2 and Systolic blood pressure (SBP) parameters have a real impact after 30 days on the neurological status in patients who have suffered from an OHCA. EtCO2 values between 30-40 mmHg, SpO2 ≥94%, and SBP between 100-130 mmHg are associated with a better neurological prognosis.
Evidence number 2
Engel et al.(11) in 2019 compared the ability of EtCO2 and Cerebral Oximetry (CerOx) to predict ROSC during resuscitation in OHCA or in the hospital emergency room.
To achieve the objective of the research, they carried out a prospective observational study in adults older than 18 years who had received CPR after suffering a non-traumatic CA. Data collection was carried out following the Utstein criteria during the period from May 16, 2010 to March 15, 2014. The parameters were measured continuously, in the case of EtCO2, through the endotracheal tube and the CerOx values using sensors on the subject’s forehead. The total number of patients evaluated was 176.
The analysis of both parameters was performed using ROC curves (AUC) and a binary logistic regression (ROSC and not ROSC), using six indicators derived from the data recorded by each device.
The authors noted that higher values and positive trends in both variables during resuscitation were positive predictors of ROSC. The indicators, average value in the last 5th, 2nd and 1st minute of CPR and the difference from the first to the last value were an acceptable predictor of ROSC for EtCO2 and an excellent predictor for CerOx.
In addition, the optimal EtCO2 value in the last two minutes of resuscitation to predict ROSC was identified, being 26.5 mmHg with a sensitivity of 74.1% and a specificity of 59.5%.
To conclude the study, it was determined that higher values and positive tendencies of capnometry and cerebral oximetry during resuscitation were associated with greater possibilities of ROSC.
Evidence number 3
In 2019 Poppe et al.(12) carried out a retrospective observational study on the value of capnography during CPR to predict ROSC and survival after 30 days, in patients who have suffered a OHCA with an underlying non-shockable rhythm.
A total of data of 2,223 victims of CA in the city of Vienna were analyzed during two years (July 2013 to August 2015). The investigation focused on 526 patients who met the following criteria: age over 18 years, non-traumatic CA with initial non-shockable rhythm, and advanced airway management during the first 15 minutes with consecutive measurement of EtCO2.
The patients finally included were divided into 3 groups according to the initial EtCO2 values (<20 mmHg, 20-45 mmHg and >45 mmHg). To compare these stratified data, the Chi square test was used. A binary logistic regression model was also performed to determine the odds ratio (OR) of any ROSC (at some point during resuscitation), sustained ROSC (until arrival at hospital), and survival after 30 days.
The results determined that initial EtCO2 values above 45 mmHg were associated with higher probabilities of ROSC [OR 2.58 (95% CI: 1.64 to 4.06); p<0.001], sustained ROSC [OR 3.59 (95% CI: 2.19 to 5.85); p<0.001] and survival after 30 days [OR 5.02 (95% CI: 2.25 to 11.23); p<0.001], when the underlying primary rhythm was asystole or pulseless electrical activity (PEA). Furthermore, levels lower than 20 mmHg were associated with a low probability of ROSC (p<0.001).
The authors concluded their study by stating that patients who have suffered OHCA with an initial non-shockable rhythm and have high initial EtCO2 values have a higher probability of sustained ROSC and survival. They also add that capnography could be used as a predictor of ROSC in these types of patients and guide decision-making regarding whether or not to continue resuscitation efforts.
Evidence number 4
Elola et al.(13) in 2019 analyzed, through a retrospective cohort study, the ability of capnography to discriminate between pulseless electrical activity (PEA) and pulsed rhythms (PR), as well as its potential to detect ROSC.
This study was carried out in a Dallas research center between 2012 and 2016. A total of 1,561 episodes of OHCA were analyzed, of which 426 were finally included when meeting the established criteria and having the parameters to evaluate available: electrocardiogram (ECG), thoracic impedance (TI) and capnography.
EtCO2 measurements were performed every minute (MEtCO2) at a 5 minute interval around ROSC (4 minutes before and 1 minute after). The results determined that EtCO2 levels were significantly higher in the cases of ROSC, with a trend from 41 mmHg (3 minutes before ROSC), to 57 mmHg in the minute after recovery.
The 3.2-second long PEA/PR segments were assessed during the chest compression-free intervals using an automatic external defibrillator (AED). In the cases of ROSC, the previous segments were labeled as PEA and those after recovery as PR. In the non-ROSC cases, all segments were labeled PEA. The detection of ROSC by the signals of the capnograph or the ECG/IT implies a good discrimination between both segments.
The results showed that the use of the three parameters together (ECG + IT + EtCO2) provides a greater discrimination of the PEA/PR segments and, therefore, a greater probability of detecting ROSC satisfactorily (AUC: 0.92). Furthermore, EtCO2 levels independently can also be considered an acceptable predictor of ROSC (AUC: 0.76).
Research demonstrates the added value of capnography in reliably detecting ROSC in patients who have suffered from an OHCA, and the authors recommend its implementation for such use.
Evidence number 5
Çalbay et al.(14) carried out an investigation in 2019 on the prognostic value of EtCO2 and different parameters in blood (pH, PO2, PCO2, lactate) in OHCA.
The objectives of this prospective cohort study were to evaluate whether EtCO2 and arterio-alveolar CO2 gradient (AaGCO2) can be used as a prognosis biomarker for ROSC. Their role in short-term neurological evaluation was also examined. Data collection was carried out from February 2016 to February 2017. The patients included were over 18 years old, admitted to the emergency room with OHCA of non-traumatic cause.
The total number of patients evaluated was 155. Resuscitation was performed according to the AHA 2015 recommendations. Arterial blood gases, EtCO2 and AaGCO2 were analyzed before and after CPR.
Regarding the results obtained, the PO2 (p=0.0006), PCO2 (p=0.0012) and AaGCO2 (p=0.0003) values at the time of admission to the emergency room, showed a statistic significant association with ROSC.
In this study, EtCO2 levels did not have a statistical significant association with ROSC (p>0.05). The mean values on arrival at the emergency service were 15.66±10.15 mmHg and in the patients who achieved ROSC, 29.48±14.98 mmHg.
In conclusion, PCO2, PO2 and AaGCO2 can be used as prognosis biomarkers for ROSC in patients in OHCA admitted to the emergency room. The parameter that showed the greatest statistical association was AaGCO2, calculated from arterial blood gas (PCO2) and capnometry (EtCO2). On the other hand, and unlike other studies, none of the parameters analyzed showed a relationship with the neurological status of the patient in the short term (p>0.05).
Evidence number 6
Javaudin et al.(15), published in 2019 a multicenter retrospective cohort study about the maximum value of EtCO2 to predict ROSC during CPR in OHCA of traumatic, cardiac and respiratory etiology.
The data for the study were extracted from “The French National OHCA Registry” (RéAC), between July 2011 and June 2018. OHCA attended by Mobile Intensive Care Units (MICU) were included. Patients under 18 years old, with ROSC before the arrival of the emergency services or who did not meet the aforementioned etiologies were excluded.
During resuscitation, the cause of the CA was assessed in situ by the physician. Capnography was continuously monitored by bag-valve-mask or through the endotracheal tube. The total number of patients evaluated was 32,249. Among them, 2,981 (9.2%) suffered from a traumatic OHCA, 12,164 (37.7%) from cardiac cause and 5,298 (16.4%) from respiratory cause. The percentage of ROSC and survival after 30 days was lower in the first group (p<0.001). The worst prognosis occurred with peak EtCO2 values during CPR of <10 mmHg.
The results regarding the mean maximum value of EtCO2 during the resuscitation of the subjects were 21.3 mmHg [95% CI (20.6–21.9)] in the OHCA of traumatic etiology, 28.0 mmHg [95% CI (27.7–28.3)] in suspected of cardiac etiology and 31.2 mmHg [95% CI (30.6–31.7)] in respiratory etiology. In the case of patients who achieved ROSC, the maximum EtCO2 values were higher; 39.4 mmHg [95% CI (38.1–40.7)], 38.4 mmHg [95% CI (37.8–38.9)] and 44.6 mmHg [95% CI (43.7–45.5)], respectively.
On the other hand, the authors analyzed the predictive value of the maximum EtCO2 value, using a ROC curve, obtaining the following AUC values for traumatic, cardiac and respiratory causes: 0.887 [95% CI (0.875–0.898)], 0.772 [95% CI 0.765– 0.780)], and 0.802 [95% CI (0.791–0.812)] respectively. The optimal EtCO2 thresholds to predict ROSC using the Youden index were also detailed, being 19 mmHg, 24 mmHg, and 28 mmHg, respectively.
The researchers concluded the study by stating that the EtCO2 peaks were higher in the subjects who achieved ROSC, regardless of the etiology of the OHCA. Likewise, this measure had a strong diagnosis value of ROSC, especially in traumatic causes. They also suggested that, given the results obtained, a single high EtCO2 value, regardless of time, could help predict ROSC, but more studies are needed to corroborate this.
DISCUSSION
In this study we wanted to update and compare the information available about the prognosis value of capnography during CPR.
Nowadays, only a few studies have discussed the impact of EtCO2 values during CPR to predict neurological status of the patient after 30 days. Some research has shown that hypocapnia is detrimental to long-term survival and prognosis; however, there is ambiguity regarding the outcomes of hypercapnia in the patient. In a meta-analysis carried out in 2016, they found that both hypocapnia (PaCO2 <35 mmHg) and hypercapnia (PaCO2 >45 mmHg) are associated with a poor prognosis, with normocapnia as the one that offers the best neurological results(16). The study by Javaudin et al.(10) also supports these results and also evaluated for the first time the optimal EtCO2 values for a better (30-40 mmHg) or worse (<20 mmHg) prognosis. They also observed that the need for inotropic support during resuscitation was an independent predictor of a poor neurological outcome. Likewise, to increase the diagnostic value of EtCO2 during CPR, they recommended its combination with other parameters such as SBP and SpO2.
During these years, research has focused mainly on analyzing static EtCO2 values to predict ROSC during CPR, which has led many authors to raise the need for additional studies evaluating dynamic trends, to better understand the role of capnography in these situations(17). In the work of Engel et al.(11) the trends of EtCO2 during resuscitation were studied using different indicators (average value last 5, 2 and 1 minute of CPR and the difference from the first to the last value), obtaining a greater ROSC prediction ability when these trends were positive and offered high EtCO2 values. Static measurements were also made: initial and maximum values, which were weaker predictors of ROSC. Furthermore, in the event that there were discrepancies in whether or not to continue with resuscitation, CerOx could be used to facilitate decision-making, since in this study it provided an excellent predictive value.
Consecutively, in the studies by Poppe et al. (12) and Javaudin et al.(15), static EtCO2 values were also analyzed: initial and maximum, respectively. In the first study, baseline values >45 mmHg were found to be associated with higher odds of ROSC when the underlying primary rhythm was asystole or pulseless electrical activity (PEA). However, in another previous review(17), initial EtCO2 values <10 mmHg were also associated with ROSC, especially in patients with a shockable initial rhythm. This leads us to consider that an initial shockable rhythm (PVT/VF) is associated with a better outcome in resuscitation, regardless of the initial EtCO2 values.
Another factor that also influences the EtCO2 values and which has not been kept in mind in most of the studies included in this review because it is not available in the databases, is the etiology of CA. Some studies have analyzed the value of EtCO2 in patients who have suffered a OHCA of cardiac or respiratory causes but, to our knowledge, no previous study has evaluated this parameter in arrests of traumatic etiology, despite representing 8% of OHCA and having a less favorable prognosis compared to other etiologies(18). Javaudin et al.(15) carried out a study where they measured the maximum EtCO2 values during the resuscitation of patients with OHCA of traumatic, cardiac and respiratory causes, finding that the maximum EtCO2 values were higher in the subjects who achieved ROSC, independently of the etiology of OHCA. However, the maximum EtCO2 values were higher in CA caused by respiratory causes, however, the predictive capacity of the capnography was greater when the cause was traumatic.
However, the limitations found in these studies must be considered. Most are retrospective, so a selection bias may have occurred due to an incomplete data record. Another weakness found is the lack of information about the ventilatory frequency during CPR. In some studies, reference is made to carrying out resuscitation following the 2015 AHA recommendations and in others it is assumed that recommendation of 10 ventilations per minute have been followed, despite not being reflected in the database. This data is very important and must be reported, since hypo or hyperventilation can give false EtCO2 measurements (falsely lower in hyperventilation and falsely high in hypoventilation)(17). The lack of a normalized ventilation rate can be a potential confounder in these studies as well as the tidal volumen (TV) given.
In the investigations carried out by Çalbay et al.(14) and Elola et al.(13), they studied different parameters that could be used, like EtCO2, as prognosis markers. In the first study, they found that the arterial gases PO2 and PCO2, obtained within 3-5 minutes after their extraction, and the AaGCO2, calculated from the same arterial blood gas and from the capnography values, offered a good predictive value of ROSC. Despite the fact that capnography did not provide a statistical significant prognosis value when it is measured independently, the authors recommended its use, since it is an easy tool to implement that does not require experience or special knowledge for its application, besides being non-invasive and low cost tool. They identify it as the most appropriate method for continuous monitoring of the patient’s clinical status during resuscitation.
In the second work carried out by Elola et al.(13), it was analyzed the predictive value that EtCO2 offers when it is added to pulse detection methods such as ECG and TI. That is the reason why, a classifier was developed based on the processing of the ECG signal, to automatically record the heart rhythms during CPR and thus be able to retrospectively evaluate the effect of the technique or treatment performed on the patient. In this case, the classifier detected two types of rhythms: PEA and PR. In addition, this instrument allows analysis of resuscitation episodes with recordings of only 3.2 seconds, which allows minimal interruption of chest compressions. The results of this study indicated that the use of capnography, together with the ECG and TI, offer greater ROSC prognosis discrimination between rhythms with and without a pulse than if they are used independently.
A notable factor in this latest investigation is the absence of data on the method used to isolate the airway. In other studies, despite having such information, patients were included regardless of the instrument used, finding a greater use of supraglottic devices(12). Nowadays, clinical studies have not reported significant differences in EtCO2 measurements offered by the endotracheal tube or laryngeal mask. A prospective study by Kannan et al.(19) found that demographic data such as sex, age and weight, as well as PO2 and EtCO2 values were comparable between both devices. This data is important to highlight regarding the possibility to recruit a greater number of participants in future studies and, on the other hand, to be considered by resuscitators.
Finally, it should be added that, as we have been able to verify both in these articles and in other reviews and meta-analysis carried out, many factors affect both the result of CPR and the values of capnography. Among them, we can highlight the etiology of the arrest and comorbidities of the patients, initiation of CPR by witnesses, quality of CPR, ventilation rate, EtCO2 measurement at different times of resuscitation, use of bicarbonate and epinephrine during CPR (EtCO2 values falsely elevated or falsely lower, respectively)(17,20). All this means that there is no clear consensus around the optimal cut-off point for EtCO2 to predict ROSC.
Currently, according to the recommendations of the AHA and the ERC of 2015, the mean EtCO2 threshold to predict ROSC is between 10-20 mmHg, but the latest studies suggest that this threshold is higher nowadays. In fact, in this review, the average value calculated from the mean EtCO2 values resulting from the different studies, which offered better results in ROSC, was approximately 28 mmHg. However, the guidelines are not yet clear, so more prospective studies would be necessary, keeping in mind potential confounders, to reach stronger conclusions.
In conclusión, the capnography values can be used in an acceptable way to predict ROSC during cardiopulmonary resuscitation; furthermore, its combination with other parameters such as CerOx, SBP, ECG or SpO2 facilitates decision-making and increases predictive capacity.
There is no consensus when determining the EtCO2 values associated with a higher or lower probability of ROSC; this is due to the use of different variable parameters (initial, maximum, mean value) and to confounding factors that increase the heterogeneity of the results.
In general, we can state that: A) Positive trends and high EtCO2 values increase the probability of ROSC and survival at discharge. In this review, the calculated average value that obtained best outcomes in ROSC was approximately 28 mmHg, a higher threshold than the one established by AHA and ERC. B) EtCO2 values <20 mmHg have been associated with a lower probability of ROSC and a worse prognosis. C) The factors that influence EtCO2 values are: the etiology of the arrest and comorbidities of the patients, initiation of CPR by witnesses, quality of CPR, initial shockable or non-shockable rhythm, ventilation rate, use of bicarbonate or epinephrine during CPR.
Conflict of interest
None
Acknowledgments
None
References
- Iglesias-Llaca F, Suárez-Gil P, Viña-Soria L, García-Castro A, Castro-Delgado R, Fente Álvarez AI, et al. Supervivencia de las paradas cardiacas extrahospitalarias atendidas por una unidad de vigilancia intensiva móvil de Asturias en 2010. Med Intensiva. 1 de diciembre de 2013;37(9):575-83.
- Grmec Š, Križmarič M, Mally Š, Koželj A, Špindler M, Lešnik B.Utstein style analysis of out-of-hospital cardiac arrest—Bystander CPR and end expired carbon dioxide. Resuscitation. 1 de marzo de 2007;72(3):404-14.
- Guidelines 2000 for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Part 6: advanced cardiovascular life support: section 7: algorithm approach to ACLS emergencies: section 7A: principles and practice of ACLS. The American Heart Association in collaboration with the International Liaison Committee on Resuscitation. Circulation. 22 de agosto de 2000;102(8 Suppl):I136-139.
- Díez-Picazo LD, Barrado-Muñoz L, Blanco-Hermo P, Barroso-Matilla S, Espinosa Ramírez S. La capnografía en los servicios de emergencia médica. SEMERGEN – Med Fam. 1 de marzo de 2009;35(3):138-43.
- Monsieurs KG, Nolan JP, Bossaert LL, Greif R, Maconochie IK, Nikolaou NI, et al. European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation. octubre de 2015;95:1-80.
- Cambra Lasaosa FJ, Pons Ódena M. Pulsioximetría y capnografía. An Pediatría. 1 de enero de 2003;59(3):259-64.
- Pantazopoulos C, Xanthos T, Pantazopoulos I, Papalois A, Kouskouni E, Iacovidou N. A Review of Carbon Dioxide Monitoring During Adult Cardiopulmonary Resuscitation. Heart Lung Circ. noviembre de 2015;24(11):1053-61.
- Tsaousi GG. The role of carbon dioxide during cardiopulmonary resuscitation. Arch Hell Med. octubre de 2017;34(5):605-14.
- Brinkrolf P, Borowski M, Metelmann C, Lukas R-P, Pidde-Küllenberg L, Bohn A. Predicting ROSC in out-of-hospital cardiac arrest using expiratory carbon dioxide concentration: Is trend-detection instead of absolute threshold values the key? Resuscitation. 2018;122:19-24.
- Javaudin F, Desce N, Le Bastard Q, De Carvalho H, Le Conte P, Escutnaire J, et al. Impact of pre-hospital vital parameters on the neurological outcome of out-of-hospital cardiac arrest: Results from the French National Cardiac Arrest Registry. Resuscitation. 2018;133:5-11.
- Engel TW, Thomas C, Medado P, Bastani A, Reed B, Millis S, et al. End tidal CO2 and cerebral oximetry for the prediction of return of spontaneous circulation during cardiopulmonary resuscitation. Resuscitation. 2019;139:174-81.
- Poppe M, Stratil P, Clodi C, Schriefl C, Nürnberger A, Magnet I, et al. Initial end-tidal carbon dioxide as a predictive factor for return of spontaneous circulation in nonshockable out-of-hospital cardiac arrest patients: A retrospective observational study. Eur J Anaesthesiol. julio de 2019;36(7):524-30.
- Elola A, Aramendi E, Irusta U, Alonso E, Lu Y, Chang MP, et al. Capnography: A support tool for the detection of return of spontaneous circulation in out-of-hospital cardiac arrest. Resuscitation. 2019;142:153-61.
- Çalbay A, Çakır Z, Bayramoğlu A. Prognostic value of blood gas parameters and end-tidal carbon dioxide values in out-of-hospital cardiopulmonary arrest patients. Turk J Med Sci. 24 de octubre de 2019;49(5):1298-302.
- Javaudin F, Her S, Le Bastard Q, De Carvalho H, Le Conte P, Baert V, et al. Maximum Value of End-Tidal Carbon Dioxide Concentrations during Resuscitation as an Indicator of Return of Spontaneous Circulation in out-of-Hospital Cardiac Arrest. Prehospital Emerg Care Off J Natl Assoc EMS Physicians Natl Assoc State EMS Dir. 31 de octubre de 2019;1-7.
- McKenzie N, Williams TA, Tohira H, Ho KM, Finn J. A systematic review and meta-analysis of the association between arterial carbon dioxide tension and outcomes after cardiac arrest. Resuscitation. 2017;111:116-26.
- Paiva EF, Paxton JH, O’Neil BJ. The use of end-tidal carbon dioxide (ETCO2) measurement to guide management of cardiac arrest: A systematic review. Resuscitation. 1 de febrero de 2018;123:1-7.
- Escutnaire J, Genin M, Babykina E, Dumont C, Javaudin F, Baert V, et al. Traumatic cardiac arrest is associated with lower survival rate vs. medical cardiac arrest – Results from the French national registry. Resuscitation. 2018;131:48-54.
- Kannan S, Harsoor SS, Sowmiya L, Nethra SS, DevikaRani D, Sathesha M. Comparison of ventilatory efficacy and airway dynamics between ProSeal laryngeal mask airway and endotracheal tube in adult patients during general anesthesia. J Anaesthesiol Clin Pharmacol. 2015;31(4):517-21.
- Hartmann SM, Farris RWD, Di Gennaro JL, Roberts JS. Systematic Review and Meta-Analysis of End-Tidal Carbon Dioxide Values Associated With Return of Spontaneous Circulation During Cardiopulmonary Resuscitation. J Intensive Care Med. octubre de 2015;30(7):426-35.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/