J Med Discov (2020); 5(4):jmd20052; DOI:10.24262/jmd.5.4.20052; Received February July 23rd, 2020, Revised August 25th, 2020, Accepted September 21st, 2020, Published October 01st, 2020.
Lessinvasive, scar less, Horizontal lateral thyroidectomy
De-bin Xu1, Shi-Min Zhuang2,*, Qian-Yi Zhong2, Liang-En Xie2, Feng pang2, Xiao-Mei Sun2
1Dept of Thyroid and Neck Surgery, The second affiliated hospital to Nan Chang University, 1 Min De Road, Nanchang, 330006, People’s Republic of China.
2Dept of Otolaryngology-Head & Neck Surgery, The Sixth Affiliated Hospital of Sun Yat-sen University, 26 Tianhe YuanChun Road, Guangzhou, Guangdong, 510655,People’s Republic of China.
* Correspondence:Shi-Min Zhuang, Department of Otolaryngology-Head & Neck Surgery, The Sixth Affiliated Hospital of Sun Yat-sen University, 26 Tianhe YuanChun Road, Guangzhou, Guangdong, 510655,People’s Republic of China. E-mail: zhuangsm05@163.com
Introduction
Thyroid cancer currently has the fastest-increasing incidence rate of all cancers in the China. The vast majority of these new cases were expected to be diagnosed among women and youngsters [1]. Advances in diagnostic and treatment techniques used in cancer management have substantially improved the prognosis and increased the life expectancy of patients with thyroid cancer. However, such techniques may lead to long-term complications, including cosmetic concerns. Improve the quality of life is a significance problem for thyroid surgeons. However, conventional open thyroidectomy leaves scars over parts of the neck, which place a great psychological burden on the patient. Thus, patients demand for minimally invasive and esthetically pleasing surgery has increased greatly. We evaluated the feasibility, safety, efficacy, and cosmetic results of horizontal lateral thyroidectomy.
Prior informed consent was obtained from patients, as was the approval of the Institutional Research Ethics Committee of the Medical Center. Patients were informed of the potential risks and benefits of horizontal lateral thyroidectomy. Preoperative evaluation included taking a clinical history and a physical examination, thyroid function tests and radiography of the thorax and ultrasonography. The ultrasonography examinations were performed by the same experienced radiologist in order to evaluate lymph node metastasis. Cases eligibility criteria were as follows: (a)Ultrasonography and computed tomography confirmed thyroid nodules and without regional lymph node metastasis. (b) The pathology of all the patients were papillary carcinoma, as indicated by fine needle aspiration cytology that was guided by high-resolution ultrasonography, and the aspiration pathology was confirmed by the surgical pathology. (c)Patients agreement with minimally invasive thyroid resection and without skin defection in the neck. Patient indifference regarding unscarred skin over the neck region or preoperatively suspected of having cervical lymph node metastasis and who underwent therapeutic lateral neck lymph node dissection were excluded from the study.
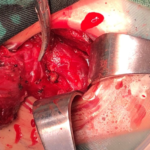
Treatment modalities.The patients were underwent the total thyroidectomy plus bilateral preventive central neck dissection group or the unilateral thyroidectomy plus isthmus thyroidectomy plus unilateral preventive central neck dissection group. The study cohort was not randomized and the decision to perform thyroidectomy was made by both the surgeon and the patients’ preoperative examination. Endotracheal intubation was performed under general anesthesia.The patient is placed in the supine position with the neck hyperextended. After conventional disinfection, a horizontal lateral incision via skin, subcutaneous tissue andplatysma was carried out above the clavicle(Fig1). Under direct vision using high frequency electrosurgical equipment separation of the platysma, loose subcutaneous connective tissue of the supraclavicular was removed. Up sides reached the above of cricoid cartilage, downward to the clavicular notch, inner sides reached the linea alba cervicalis(Fig2). The anterior neck muscles were blunt dissection from the inner side of the sternocleidomastoid muscle and protect the sternocleidomastoid muscle. The lateral thyroid vein was coagulated and cut using a harmonic scalpel. The inferior thyroid artery and, afterwards, the superior thyroid artery were with the harmonic scalpel. The thyroid lobe was separated from the trachea and the thyroid suspensory ligament and finally the inferior blood supply were severed.The thyroid isthmus and lateral lobes removed while preserving both parathyroid glands and the recurrent laryngeal nerve(Fig3,4). During the procedure, the surgeon should be careful to avoid injury to thesuperior laryngeal nerve, recurrent laryngeal nerve, trachea, and parathyroid, and the ultrasonicscalpel should be maneuvered carefully to avoidheat damage.
Fig.1 horizontal lateral incisionAnatomical location
Fig.2 separation of platysma myocutaneous fla
Fig.3 exposed and protected the recurrent laryngeal nerve,exposed and protected the parathyroid
Fig.4 Intradermal suture cosmetic
Node clearance was performed cranially to both superior thyroid arteries and the pyramidal lobe, caudally to the innominate vein, laterally to the carotid sheaths and dorsally to the prevertebral fascia [3]. There was an drainage tube left. The skin was closed with intracutaneous5.0 absorbable colourless monocryl suture.
Results
All lesions were completely resection. There were no intra-or postoperative complications. Both voice folds were adequately mobile on the ENT assessment on the first postoperative day. All patients postoperative stay after horizontal lateral thyroidectomy were significantly shorter and none of temporary recurrent laryngeal palsy, and the final pathology report provided the diagnosis of papillary thyroid carcinoma.All patients follow-up six to twelve months after the procedure, and underwent high-resolution ultrasonographyand radiographic imaging.The remaining glandswere echo uniform. No obvious space-occupyinglesions or calcifications were seen. No abnormalities were visible around the original site of thethyroid gland, confirming complete excision with no residual disease. The scar above the clavicle was barely visible (Fig5).
Fig.5 One month after surgery
Discussion
The advantages of all minimally invasive procedures are similar, including reduced postoperative pain, smaller blood loss, and faster social reintegration [2-4]. In thyroid surgery, more and more operations are being performed of invasive approach versus traditional is a better cosmetic effect [2, 3,5-9]. The majority of patients with thyroid disorders are women.Traditionally, the thyroidectomy incision is made in the visible, uncovered area of the neck. Beside, cause of poor cosmetic after conventional thyroidectomy is a scar that moves during swallowing due toadhesion of the platysma to the skin and the front neck muscles after a large dissection of tissues. After the horizontal lateral thyroidectomy surgery, there are no adhesions betweenthe scar and the front neck muscles, because anatomical advantage of this approach, we canavoid to dissect strap mucle. There are alsoreduced sensory disturbances and discomfort in theneck in comparison to traditional thyroidectomy [10,11]. The incision hidden in the supraclavicular area that is usually covered with clothes further improves the cosmetic effect of the horizontal lateral thyroidectomy.
For horizontal lateral thyroidectomy surgery to become accepted as a standard option for thyroid procedure, the surgery should be safe, not require specialized surgical skills, result in patient satisfaction, and provide the same or similar long-term prognosis as other types of surgery[11].A clinical evaluation was made of the thyroid surgery based on the results of thyroid operations performed and the questionnaire compiled from patients. We found that horizontal lateral thyroidectomy surgery offered more than simple cosmetic advantages. We must take into consideration the fact that many of the patients who underwent conventional surgery had larger tumors, which required larger-scale surgery, resulting in more complaints than horizontal lateral thyroidectomy surgery. In addition, more women underwent horizontal lateral thyroidectomy surgery than conventional surgery. However, it should be noted that patient satisfaction was no lower after horizontal lateral thyroidectomy surgery than after conventional surgery. Furthermore, horizontal lateral thyroidectomy surgery requires a shorter postoperative stay. Even though the same clinical pathway is used, regardless of the surgical method the postoperative stay after horizontal lateral thyroidectomy surgery was significantly shorter than that after conventional surgery, which could also contribute to the low number of complaints. After horizontal lateral thyroidectomy surgery, the patients were less worried about the scar and more relaxed overall, which consequently resulted in an earlier discharge.
All these factors seem to account for the higher satisfaction. In regard to safety, there is much less bleeding in horizontal lateral thyroidectomy surgery than in conventional surgery. On the other hand, horizontal lateral thyroidectomy surgery presents different challenges, not least of which is the operative time involved. In our hospital, the conventional method is now used only for large tumors, so the average operative time is longer than that for a regular operation. However, horizontal lateral thyroidectomy surgery takes less time than this. Another consideration is the postoperative development of temporary recurrent laryngeal palsy, which was none of our patients who underwent horizontal lateral thyroidectomy surgery. Considering that the location of the recurrent laryngeal nerve is carefully checked during surgery, regardless of the method used, it should be easier to locate with horizontal lateral thyroidectomy surgery because provides an enlarged and erthyphoria view.Several measures could be taken to overcome laryngeal palsy, such as not using the ultrasonically activated scalpel near the recurrent laryngeal nerve, and ensuring there is a sufficiently large field of vision.
Conclusions
Thyroid lobectomy performed with horizontal lateral thyroidectomy surgery via the above the clavicle area that is usually covered with clothes is feasible and provides a good cosmetic effect in carefully selected patients.
Conflict of interest
We declare no conflicts of interest.
Acknowledgments
This study is supported by the Science and technology of Jiangxi province(20195220), and education and technology of Jiangxi province(190153).
References
- Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. RevisedAmerican Thyroid Association management guidelines for patients withthyroid nodules and differentiated thyroid cancer. Thyroid 2009;19:1167-214.
- Ohgami M, Ishii S, Arisawa Y, et al. Scarless endoscopic thyroidectomy: breast approach for better cosmesis. Surg LaparoscEndosc Percutan Tech 2000; 10: 1-4.
- Jiang Z, Zhang W, Jiang D, et al. Clinical benefits of scarless endoscopic thyroidectomy: an expert‘s experience. World J Surg2010; 35: 553-7.
- Cho YU, Park IJ, Choi KH, et al. Gasless endoscopic thyroidectomyvia an anterior chest wall approach using a flap-lifting system.Yonsei Med J 2007; 48: 480-7.
- Ikeda Y, Takami H, Sasaki Y, et al. Endoscopic neck surgery by theaxillary approach. J Am Coll Surg 2000; 191: 336-40.
- Liu S, Qiu M, Jiang DZ, et al. The learning curve for endoscopicthyroidectomy: a single surgeon‘s experience. Surg Endosc2009; 23: 1802-6.
- Slotema ET, Sebag F, Henry JF. What is the evidence for endoscopic thyroidectomy in the management of benign thyroid disease? World J Surg 2008; 32: 1325-32.
- Bellantone R, Lombardi CP, Bossola M, et al. Video-assisted vsconventional thyroid lobectomy – a randomised trial. Arch Surg2002; 137: 301-4.
- Lombardi CP, Raffaelli M, Princi P, et al. Safety of video-assistedthyroidectomy versus conventional surgery. Head Neck 2005; 27:58-64.
- Ikeda Y, Takami H, Sasaki Y, et al. Comparative study of thyroidectomies. Endoscopic surgery versus conventional open surgery. Surg Endosc 2002; 16: 1741-5.
- Ikeda Y, Takami H, Sasaki Y, et al. Clinical benefits in endoscopicthyroidectomy by the axillary approach. J Am Coll Surg 2003; 196:189-95.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/