J Med Discov (2020); 5(2):jmd20010; DOI:10.24262/jmd.5.2.20010; Received February 16th, 2020, Revised April 17th, 2020, Accepted April 23rd, 2020 , Published April 28th, 2020.
Giant Cavernous Hemangioma of the Skull Vault
Leonardo Furtado Freitas1, Daniela Cardinal de Vasconcellos2,*, Christiane Monteiro Siqueira Campos1, Victor Hugo Rocha Marussi1, Lazaro Luis Faria do Amaral3, Paulo Marcio Porto de Melo4, Rafael Duarte de Souza Loduca4
1Beneficência Portuguesa Hospital of São Paulo, São Paulo-SP, Brazil.
2Neuroradiology at Diagnósticos da América S.A., São Paulo-SP, Brazil.
3Beneficência Portuguesa Hospital of São Paulo, São Paulo-SP, Brazil.
4Hospital das Forças Armadas, São Paulo-SP, Brazil.
* Correspondence: Daniela Cardinal de Vasconcellos,Neuroradiology at Diagnósticos da América S.A., São Paulo-SP, Brazil. Email: danielacardinal@hotmail.com
Abstract
Abstract Primary skull intraosseous cavernous hemangiomas are rare benign vascular tumors that account for about 0.2% of all bone tumors and 10% of benign skull tumors. These tumors typically present as well delimited osteolytic lesions in the calvary, however giant and ossified hemangioma has rarely been reported in the literature. Total surgical excision is the treatment of choice and the prognosis after complete excision is excellent, with recurrence usually rare. The following is a rare case of giant skullcap hemangioma with discussion of the pathology, imaging, differential diagnoses and treatment of this entity.
Keywords: ihemangioma, cavernous, cap
Introduction
Primary intraosseous cavernous hemangiomas of the skull are rare benign vascular tumors representing about 0.2% of all bone tumors and 10% of benign skull tumors (1,2). They are most commonly found in the 4th and 5th decades of life, with higher incidence in females. These tumors typically present as well delimited osteolytic lesions in the calvary, however giant and ossified hemangioma has rarely been reported in the literature. Total surgical excision is the treatment of choice and the prognosis after complete excision is excellent and recurrence is generally rare (1,2,3). The following is a rare case of giant skullcap hemangioma with discussion of the pathology, imaging, differential diagnoses and treatment of this entity.
Case Report
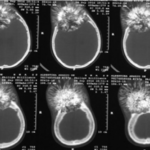
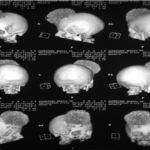
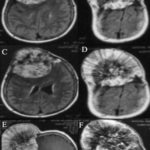
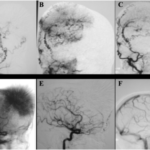
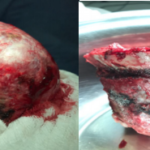
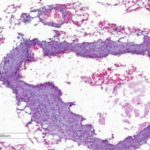
Female patient, 60 years old, with headache and painless progressive bulging of the skull vault. The radiograph of the skull showed a large sclerotic mass with spiculated contours in the right frontal region (Figure 1). Cranio-brain computed tomography allowed the characterization of a large ossified mass of spiculated contours and a component of permeate fat in the frontal region, especially on the right (Figures 2 and 3). Brain magnetic resonance showed a lesion with heterogeneous impregnation and signal at T1, T2 and FLAIR (Figures 4 and 5). Digital cerebral angiography was also performed, noting the lesion blush and blood supply from branches of the right external carotid artery (Figure 6). The patient underwent surgery and the mass was completely excised (Figure 7). Histopathological examination showed dilated blood vessels interspersed with fibrous tissue (Figure 8), findings compatible with cavernous hemangioma.
Fig. 1: Skull X-Ray - volumous sclerotic and spiculated mass in the frontal bone, predominantly at right side.
Fig. 2: Brain computed tomography with bone window - volumous ossified mass with spiculated contours in the frontal bone, predominantly at right side, with thinning and remodeling of the inner table, suggesting a slow growing process.
Fig. 3: Brain computed tomography with brain window – showing a fatty component among the lesion.
Fig. 4: Brain magnetic resonance with 3D Volume Rendering reconstruction showing a volumous mass with spiculated contours in the frontal bone.
Fig. 5: Brain magnetic resonance showing a volumous mass with spiculated contours in the frontal bone and T2 and FLAIR hyperintensity, with prominent and heterogeneous enhancement, causing extrinsic compression of the cerebral parenchyma. Aand B axial slices ponderated in T2. C and D axial slices in FLAIR. E and F , T1 post contrast sagittal and axial slices.
Fig. 6: Cerebral angiography showing lesion”blush" and vascularization from right external carotid artery branches. Cateterization of the external carotid artery (A, B and C). Cateterization of the right carotid artery (D, E and F).
Fig. 7: Macroscopy - complete excision of the mass after surgical intervention.
Fig. 8: Anatomopathological exam (HE – hematoxiline-eosine) - dilated small vessels, wuth thin walls, marginated by fibrous tissue.
Discussion
Primary intraosseous cavernous hemangiomas of the skull are rare benign vascular tumors that represent about 0.2% of all bone tumors and 10% of benign skull tumors (1,2). They occur most commonly in the spine and rarely in the skull². The frontal and parietal bones are the most frequently involved sites in the skullcap (2,3). Hemangioma can be classified histologically into 3 types: cavernous, capillary and mixed. Cavernous hemangioma consists of dilated blood vessel clusters that are separated by fibrous septa, while capillaries are rich in small vessels without many interposed fibrous septa. Most skull hemangiomas are cavernous, while vertebral hemangiomas are usually capillary ².
Fig. 9: Patient before and after surgical intervention.
These lesions can be found in all age groups, being more common in the fourth and fifth decades of life and are predominantly female with a ratio of 2: 1 to 4: 1 (2,3,4). They arise from vessels in the diplomatic space from branches of the external carotid artery. Although the pathogenesis remains unknown, some authors have proposed a hereditary nature for “vascular malformations” of the calotra as autosomal recessive inheritance. Others have indicated that proliferation and differentiation of primitive mesenchymal cells.
Undifferentiated disorders induced by a variety of stimuli may be the potential etiology². Trauma may also be an important etiology, according to some cases reported in the literature².
They are usually asymptomatic lesions, however when they reach large dimensions they manifest as a hard, palpable and slow growing mass. Neurological deficit is uncommon because these tumors tend to expand externally rather than internally, although intracranial expansion has been reported 4.
Radiological evaluation includes simple skull radiographs, computed tomography (CT) and magnetic resonance imaging (MRI) ². CT is an excellent evaluation method because it allows detailed characterization of cortical and trabecular bone, as well as involvement of adjacent soft tissues. Although the appearance on CT may vary, the most common finding is an osteolytic expansive lesion, with thin and sclerotic edges, which maintains the integrity of the inner and outer bone boards (1,2). They may also have internal components and sunburst edges ¹. Large and ossified lesions have rarely been described in the literature. The intensity of the MR signal depends on the venous stasis in the dilated blood vessels and also on the amount of adipose tissue present in the bone marrow. Although T1-weighted sequences may show high or low intensity signals, water-sensitive sequences, such as T2 and FLAIR, generally exhibit hypersignal due to slow blood flow. Cavernous hemangioma typically presents intense enhancement to paramagnetic contrast.
Differential diagnoses for intradiploic expansive lesions include metastases, intraosseous meningiomas, sarcomas, Langerhans cell histiocytosis, eosinophilic granulomas, fibrous dysplasia, giant cell tumors, aneurysmal bone cysts, osteomas, Paget’s disease, and others (1,2). . Imaging characteristics are not specific, preoperative diagnosis is difficult and histopathology is essential.
Complete surgical resection is the treatment of choice, emphasizing the importance of a normal bone margin to reduce the risk of bleeding (1,2). Cavernous hemangiomas should be considered as a differential diagnosis even in completely ossified calvary masses and an adequate preparation to minimize blood loss, such as embolization, may be considered². Recurrence is rare.
In conclusion, primary intraosseous cavernous hemangiomas of the skull are rare benign lesions of vascular origin, showing imaging findings similar to many other bone lesions, and are difficult to distinguish, although the characterization of signs of slow growth (surrounding bone remodeling), foci of permeate fat and spiculated central and marginal aspects, unlike osteosarcomas, for example, in which the periosteal reaction that assumes this aspect may guide the diagnostic reasoning, and the histopathological examination remains the “gold standard”. Total resection with non-compromised bone margins is the treatment of choice, with excellent prognosis and generally rare recurrence.
Conflict of interest
None
Acknowledgments
None
References
- Tyagi DK, Balasubramaniam S, Sawant HV. Giant primary ossified cavernous hemangioma of the skull in an adult: A rare calvarial tumor. Journal of Neurosciences of rural pratice. Jul-Dec 2011; 2(2):174-177.
- Yang Y, Guan J, Ma M, Li Y, Xing B, Ren Z. et al. Primary Intraosseus Cavernous Hemangioma in the Skull. Medicine. Marc 2016; 95(11):1-12.
- Nair P, Srivastava KA, Kumar R, Jain K, Sahu RN, Vij M, et al. Giant primary Intraosseus Calvarial Occipital Bone. Neurology India. Sep-Oct 2011; 59: 775-777.
- Park, BH, Hwang E, Kim CH. Primary Intraosseous Hemangioma in the Frontal Bone. Archive of Plastic Surgery. Mayo 2013; 40(3):283-285.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/