J Med Discov (2019); 4(4):jmd19021; DOI:10.24262/jmd.4.4.19021; Received June 28th, 2019, Revised September 20th, 2019, Accepted October 20th, 2019, Published October 30th, 2019.
Atypical presentation of CMV meningoencephalitis in an immunocompetent patient
André Luiz Guimarães de Queiroz, MD¹,*, Karlla Danielle Ferreira Lima, MD¹, Hennan Salzedas Teixeira, MD¹, Carmen Lucia Penteado Lancellotti MD, PHD³, Leonardo Furtado Freitas, MD², Márcio Luiz Escorcio Bezerra, MD, PHD¹, Alex Machado Baêta, MD, PHD¹
1Neurology Departments, Hospital BP – Beneficência Portuguesa de São Paulo, Brazil.
2Neuroradiology Departments, Hospital BP – Beneficência Portuguesa de São Paulo, Brazil.
3Neuropathology Departments, Hospital BP – Beneficência Portuguesa de São Paulo, Brazil.
* Correspondence: Dr. André Luiz Guimarães de Queiroz, Beneficência Portuguesa Hospital, 769 Maestro Cardim St., São Paulo, SP Brazil. e-mail: andreqz@gmail.com
Abstract
Cytomegalovirus (CMV) is a DNA virus which usually causes asymptomatic infections in immunocompetent patients. The involvement of the central nervous system (CNS) by CMV in immunocompetent adults is rare. Our study concerns a case of CMV encephalitis in an adult female who was diagnosed by brain biopsy. Remarkably, the patient starts with a meningitis presentation who got better and later presented clinical signs of acute encephalitis.
Keywords: Cytomegalovirus, Meningoencephalitis
Introduction
Cytomegalovirus (CMV) is a DNA virus which usually causes asymptomatic infections in immunocompetent patients [1,2]. In symptomatic infections, the most common clinical presentation is that of a mononucleosic syndrome. The involvement of the central nervous system (CNS) by CMV in immunocompetent adults is exceptional, with few references in the literature, let alone with anatomo-pathological evidence of the disease [3,4]. CMV infection can induce neurological syndromes with different manifestations (CMV infection include encephalitis, ventriculitis, myelitis, retinitis, radiculoganglionitis, and peripheral neuropathies) [5]. Encephalitis is a rare manifestation with a difficult diagnose which depends on clinical, imaging, and laboratory criteria. CMV encephalitis primarily affects immunocompromised patients, such as those with HIV/AIDS, transplant recipients on immunosuppressive therapy, and those with a malignant hematological disease. In the past, only a few cases of CMV encephalitis have been described in patients not belonging to these groups [6,7]. Our study concerns a case of CMV encephalitis in an adult female who was diagnosed by brain biopsy. Remarkably, the patient starts with a meniningitis presentation who got better and later presented clinical signs of acute encephalitis.
Case Report
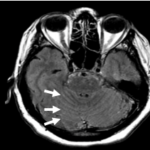
A 62-year-old woman with 2-week-long headache and disorientation. The medical history was constituted by Non-Hodgkin’s Lymphoma that went into remission about 10 years earlier, type-2 diabetes and hypertension. The confusion progressed and the patient experienced memory impairment and psychomotor agitation. Neurological examination did not show meningeal signs or focal deficits. General blood tests were all normal. Negative HIV test and negative tumor markers with no other evidence of immunologic impairment. Initial lumbar puncture revealed white blood cell count of 616 cells/mm3 (59% lymphocytes, 30% monocytes and 3% neutrophils), protein 177 mg/dL and glucose 32 mg/dL (simultaneous blood glucose level of 154 mg/dL). Brain MRI suggest a leptomeningeal inflammatory process (Fig. 1). A lumbar puncture was repeated 28 days after the first one, showing cellularity reduction (160 cells/mm3, glucose level 38 mg/dL and protein level 98 mg/dL). Cerebrospinal fluid analysis (CSF) was sent for detection and quantification of human polyomavirus BK as well as for viral cultures, the results were negative as well as the flow cytometry immunophenotypic for evaluation of CNS neoplastic cells. Patient progresses with gradual improvement and was discharged with weekly control CSF and outpatient care. One month later, the patient experienced again psychomotor agitation, confusion, altered mental status and mild dysarthria. A new MRI showed significant reduction of the anomalous leptomeningeal contrast impregnation.
Fig.1 Post-contrast FLAIR MRI sequence showing impregnation in the internal auditory conducts (red arrows), in the sulci between the cerebellar folia (white arrows) and in the interpeduncular cistern (arrowhead), compatible with inflammatory / infectious process (leptomeningitis).
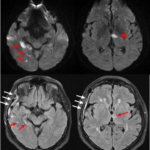
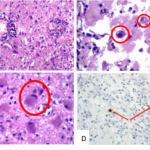
Although it has been a characterization of multiple foci of cytotoxic edema in a corticossubcortical situation in the left inferior parietal lobe, temporal lobe and in the mesial occipitotemporal transition on the right, in the thalamus and in the postero-inferior and antero-superior aspects of the right cerebellar hemisphere, which should represent ischemia due to infectious vascular compromise (Fig 2.). CSF analysis was repeated on day 28, 74, 91 and day 110, showing a progressive cellularity improvement (last one with 30 cells/mm3). A biopsy from the temporal lesion was performed. Histopathology revealed necrotizing meningoencephalitis with intense inflammatory activity, with cytopathic effects caused by CMV virus, confirmed by immunohistochemistry (Fig. 3). The patient started with intravenous treatment that consisted on taking ganciclovir at 5 mg / kg IV every 6 hours for a total of 2 weeks, then the treatment was completed with 3 months of oral ganciclovir. Achieving significant clinical and imaging improvement.
Discussion
CMV encephalitis occurs very rarely in immunocompetent adults and does not seem to be associated with a defined clinical syndrome [8]. Therefore, diagnosis depends on intrathecal or histopathologic evidence of CMV infection. The low sensitivity of virus culture techniques made this diagnosis very difficult. Diagnosis of CMV encephalitis was based on a brain biopsy and not by amplification of virus-specific DNA fragments from CSF. Virus-specific antigen and DNA could be detected in PBL by the APAAP technique, centrifugation culture, and PCR. Absence of any detectable CMV-specific antibodies may indicate a primary CMV infection.
Fig. 2 (A) Diffusion sequence demonstrating multiple restricted areas in the right occipital and temporal lobes (arrows) and in the ventromedial aspect of the left thalamus (arrowhead), compatible with acute ischemia related to secondary vasculitis; (B) FLAIR sequence demonstrating post-operative status in the right skull cap for brain biopsy (yellow arrows) and sequelae of gliosis due to prior ischemia (red arrows).
Fig. 3 (A) Perivascular inflammatory infiltrate. HEX200; (B) and (C) Cytopathic effects with intranuclear basophilic inclusion; (D) Immunohistochemistry showing Cytomegalovirus CCH2+DDG9 Clone (Dako). IHCX100. Conclusion of a Necrotizing meningoencephalitis with intense inflammatory CMV activity.
The lack of CSF findings and variable clinical presentation makes the CMV encephalitis diagnosis often difficult. This disorder is usually described as monophasic and self-limited with favorable outcome in immunocompetent patients [9]. An interesting and unusual observations in our patient was that CMV infections involving the central nervous system are uncommon in previously healthy individuals, and, whilst meningitis findings were improving in CSF analysis, isolated CMV parenchymal lesions were emerging. Until now, this clinical presentation was never presented on case reports before.
In our case, the patient presented a predominant clinical picture of subacute meningitis, with partial improvement of the abnormalities in the cerebrospinal fluid. After 2 months, the patient evolved with psychomotor agitation and confusion, with clinical and radiological signs of encephalitis, evidencing a biphasic case, different from the natural evolution of the disease described in the literature in immunocompetent CMV infected patients.
Conflict of interest
None
Acknowledgments
None
References
- Vinters HV, Kwok MK, Ho HW, et al. Cytomegalovirus in the nervous system of patients with the acquired immune deficiency syndrome. Brain. 1989;112:245-268.
- Coyle PK. Acquired cytomegalovirus. In Gilman S, Goldstein G, Waxman S (eds). Neurobase [cd-rom], 2.Ed. Yale University, 1999.
- Ho M. Cytomegalovirus: biology and infection. 2.Ed. New York: Plenum, 1991.
- Griffiths PD, McLaughlin JE. Cytomegalovirus. In Scheld WM, Whitley RJ, Durack DT (eds). Infections of the central nervous system. 2 Ed. Philadelphia: Lippincott–Raven, 1997:107-115.
- Griffiths P., Cytomegalovirus infection of the central nervous system. Herpes. 2004;11 Suppl 2:95A-104A.
- Arribas JR, Storch GA, Clifford DB, Tselis AC. Cytomegalovirus Encephalitis. Ann Intern Med 1996;125:577–87.
- Micallef S, Galea R. CMV encephalitis in an immune-competent patient. BMJ Case Rep 2018;546–9.
- Prösch S, Schielke E, Reip A, et al. Human cytomegalovirus (HCMV) encephalitis in an immunocompetent young person and diagnostic reliability of HCMV DNA PCR using cerebrospinal fluid of nonimmunosuppressed patients. J Clin Microbiol. 1998;36(12):3636–3640.
- Rafailidis PI, Mourtzoukou EG, Varbobitis IC, Falagas ME. Severe cytomegalovirus infection in apparently immunocompetent patients: a systematic review. Virol J. 2008;5:47.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/