J Med Discov (2019); 4(3):jmd19025; DOI:10.24262/jmd.4.3.19025; Received July 24th, 2019, Revised August 14th, 2019, Accepted August 23rd, 2019, Published August 30th, 2019.
Patient with lung adenocarcinoma has a survival rate of 12+ years
Javier Corral1, Zeinab Abdulrahman1, Hayder Azeez1,*
1Internal medicine department at Texas Tech University Health Sciences Center El Paso, 4800 Alberta Avenue, El Paso, TX 79905
* Correspondence: Javier Corral, Texas Tech University Health sciences Center EL Paso, Internal medicine department, 4800 Alberta Avenue, El Paso, Texas 79905. Email: Javier.corral@ttuhsc.edu.
Abstract
We describe a case of an unusual presentation and survival rate of lung adenocarcinoma, stage IIIB in a nonsmoker Hispanic female. Lung adenocarcinomas are common in Asian women, and it is rare in Hispanics. Once the malignancy was diagnosed and the metastasis was excluded, treatment with a usual dose of Erlotinib was started. Afterward because of the side effect of the medication we kept the patient on an unusually low dose of Erlotinib, followed by an obvious diminution in the primary tumor showed by CT scan. The patient is still surviving for 12 + years.
Keywords: Lung adenocarcinoma in Hispanic, Scalp rash, Tyrosine kinase inhibitor (Erlotinib)
Introduction
Non-small cell lung cancer accounts for 80 percent of lung malignancies. Histologically, lung adenocarcinoma (AC) accounts for most of the non-small cancer and is the most common one among nonsmokers.[1,2] Lung adenocarcinoma is common in Asian women, people under the age of 45 and it is rare in Hispanics.[3] The 5 years survival rate for stage IIIB adenocarcinoma is about 26%.[4]
Non–small cell lung cancer is often asymptomatic at diagnosis and may be found incidentally on imaging performed for other reasons. If symptoms are present, they are often related to the specific locations of tumor masses and the occurrence of paraneoplastic syndromes. The symptoms of centrally located lesions include cough, hemoptysis, wheezing, stridor, dyspnea, and post obstructive pneumonia. Peripheral lesions can cause pain due to pleural or chest wall invasion, cough, or restrictive dyspnea.[5] CT scanning is an integral part of the assessment of patients with lung cancer. Chest CT scans should also include the upper abdomen to assess two of the most common sites of metastases (liver and adrenal glands).[6] The International Society for the Study of Lung Cancer (IASLC) published a histological classification of lung adenocarcinomas in 2011.[3] The main interest of such classification is its prognostic value since histological type is closely associated with clinical, pathological and molecular parameters.[7,8]
Invasive lung adenocarcinoma, which is the most common of cancer is divided into five groups based on growth pattern and/or shape of a tumor. These are: lepidic, acinar, papillary, micropapillary and solid. Of these micropapillary-predominent adenocarcinomas were added as a new histological subtype and has been reported as an aggressive variant of adenocarcinoma with a poor prognosis.[9]
In more than 90% of lung adenocarcinomas cases, two or more components exist, for which reason the prognosis of lung AC varies based on the proportion of each histopathological component.[10] In addition to histological pattern, the staging also drives the prognosis of lung cancer with the presence of metastasis inflicting the most negative factors. For this reason, it is very important to confirm or exclude the presence of metastasis immediately after a diagnosis is known.
In lung cancer, Erlotinib is effective in patients with or without EGFR mutation but appears to be more effective in patients with EGFR mutation.[11]
However, we would like to present our case that doesn’t follow the usual presentation and survival rate.
Case Presentation
In April 2007, a 69-years old nonsmoking Hispanic woman without past medical history presented herself to a family medicine physician after she noticed a lump in the left side of her neck for four months, increase in size. She denied loss of weight, loss of appetite, fever, cough, diarrhea, constipation. Significant physical findings are multiple adenopathies in the left side of the neck, in supraclavicular area, mobile, no tenderness, not fix, the biggest one is four centimeters.
In May 2017 the patient was referred to our Institution (the internal medicine department at Texas Tech University Health Sciences Center clinic) for further evaluation. In May of 2007, a chest computed tomography (CT) scan without contrast revealed a 1.8 cm spiculated nodule in the right upper lobe associated with mediastinal and contralateral supraclavicular adenopathy suggestive of primary lung neoplasm. To further investigate this finding, a CT guided needle core biopsy showed poorly differentiated invasive adenocarcinoma, the focal peripheral bronchioloalveolar pattern is present. Immunohistochemistry showed that the tumor cells were positive for cytokeratin 7, negative for cytokeratin 20, positive for TTF1, and Ki67 (proliferation rate) was low, PAS is positive in tumor cells. Bilateral mammogram and breast ultrasound were normal, they didn’t show any evidence of malignancy in the breast.
CT scan without the contrast of the abdomen and pelvis was done, it didn’t show any further metastasis. A Positron emission tomography/computerized tomography (PET/CT) scan excluded additional disease localization, as PET imaging showed hypermetabolic activity in a 10 mm retrocaval/paratracheal node with SUVs peaking at 4.8. A 15 mm premarital node hypermetabolic activity with SUV peaking at 9.6. Uptake in the right hilum shows SUVs peaking at 5.1. These findings are associated with hypermetabolic mass in right mid lung zone at the level of the middle lobe bronchus. Inspection of the musculoskeletal system shows no convincing PET evidence for bony sites of malignancy. Therefore, a clinical diagnosis of lung adenocarcinoma was made, the lung adenocarcinoma was determined to be clinical stage IIIB (cT1b, cN3, M0).
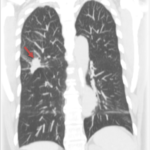
The patient was treated with six cycles of Taxol/Carboplatin. Five months later, a CT scan identified persistent and large pre-tracheal and left supraclavicular lymph nodes. The radiological response was evaluated as stable disease. Testing for EGFR mutations at that time was in its infancy stage, therefore identifying EGFR mutations was not critical to inform treatment decisions.[12-14] Subsequently, the patient was started on second-line therapy with Erlotinib 150mg daily on Nov 2007. She showed a good response indicated by CT scan without contrast in May 06, 2008 as It revealed no evidence of mediastinal adenopathy only sub-centimeter lymph nodes in the left supraclavicular region and in the paratracheal space that have not changed in size or characteristics, persistent spiculated lesion in the right upper lobe that has not changed in size or character in relation to the previous study.
On Jan 2012 the patient developed a scalp rash as a side effect of Erlotinib, therefore the dosage was reduced to 100 mg, afterward, the patient still complained from the rash and the pruritus of the body and the scalp, so the dose was reduced to 50 mg on Jan of 2015. Currently Patient is on 50 mg of Erlotinib with no progression or new mass in prospective CT scan. The patient has 12+ years of survival with stage IIIB lung adenocarcinoma.
Fig. 1 A coronal CT scan in 2007, revealed right upper lobe lung mass (arrow).
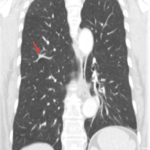
Fig. 2 A coronal CT scan in 2017, after 10 years of therapy showed minimal scar tissue in the right upper lobe, which is considered as a complete resolution (arrow).
Fig. 3 An axial section of a CT scan in 2007 showing a 19.3 mm mass in the left supraclavicular area consistent with lymph node metastasis (arrow).
Fig.4 An axial section of a CT scan in 2017 showing a complete resolution of lymph node metastasis (arrow).
Results
Although Lung adenocarcinoma is less common in the Hispanic population and has a medium survival rate, our patient has survived for 12+ years with a diagnosis of lung invasive adenocarcinoma (T1bN3M0). Currently, the patient remains on oncological follow-up visit, in October 2017, CT scan showed stable 1 cm spiculated nodule in the posterior segment of the right upper lobe. No new lung nodules or lung mass. In October 2018, (PET/CT) scan showed no scintigraphy evidence of osteoblastic metastatic disease.
Conclusion
In general, it is commonly known in the medical literature that overall survival expectancy for patients with stage IIIB Lung adenocarcinoma is in the ballpark of 12.6 months.[15,16] Our case is a unique case presentation, as she has been living for more than 12 years with a nonstandard dose (50 mg) of Erlotinib alone. Most recent CT scan in July of 2017 showed minimal scar tissue, which is considered as a complete resolution. As a result, an obvious diminution in the primary tumor and a remarkable reduction in the patient’s tumor burden were observed which indicated good control of cancer itself is possible in this case. Unfortunately, the immunohistochemistry pictures for the tumor cells and the tissue were unable to be retrieved for genomic testing as the hospital usually discard all tissues and immunohistochemistry pictures after 10 years.
Conflict of interest
The authors declare that they have no competing interests.
Acknowledgments
No funding has been received for the study.
References
1 Ma NQ, Liu LL, Min J, Wang JW, Jiang WF, Liu Y, et al. The effect of down regulation of calcineurin Aalpha by lentiviral vector-mediated RNAi on the biological behavior of small-cell lung cancer and its bone metastasis. Clin Exp Metastasis. 2011; 28: 765-78.
2 Khuder SA. Effect of cigarette smoking on major histological types of lung cancer: a meta-analysis. Lung Cancer. 2001; 31: 139-48.
3 @NCICancerStats. Cancer of the Lung and Bronchus – Cancer Stat Facts. 2019.
4 Goldstraw P, Chansky K, Crowley J, Rami-Porta R, Asamura H, Eberhardt WE, et al. The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J Thorac Oncol. 2016; 11: 39-51.
5 Diniz Gomes DB, Gold KA, Gibbons DL, Eapen CGA. Non–Small Cell Lung Cancer. In: Kantarjian HM, Wolff RA (eds.). The MD Anderson Manual of Medical Oncology, 3e. New York, NY: McGraw-Hill Medical 2016.
6 Deatrick KB, Long J, Chang AC. Thoracic Wall, Pleura, Mediastinum, & Lung. In: Doherty GM (ed.). CURRENT Diagnosis & Treatment: Surgery, 14e. New York, NY: McGraw-Hill Education 2015.
7 Mansuet-Lupo A, Bobbio A, Blons H, Becht E, Ouakrim H, Didelot A, et al. The new histologic classification of lung primary adenocarcinoma subtypes is a reliable prognostic marker and identifies tumors with different mutation status: the experience of a French cohort. Chest. 2014; 146: 633-43.
8 Chen Z, Liu X, Zhao J, Yang H, Teng X. Correlation of EGFR mutation and histological subtype according to the IASLC/ATS/ERS classification of lung adenocarcinoma. Int J Clin Exp Pathol. 2014; 7: 8039-45.
9 De Oliveira Duarte Achcar R, Nikiforova MN, Yousem SA. Micropapillary Lung Adenocarcinoma: EGFR, K-ras, and BRAF Mutational Profile. American Journal of Clinical Pathology. 2009; 131: 694-700.
10 Moon Y, Sung SW, Lee KY, Kim YK, Park JK.
11 Sekhon N, Kumbla RA, Mita M. Chapter 1 – Current Trends in Cancer Therapy. In: Gottlieb RA, Mehta PK (eds.). Cardio-Oncology. Boston: Academic Press 2017; 1-24.
12 Wu YL, Zhou C, Hu CP, Feng J, Lu S, Huang Y, et al. Afatinib versus cisplatin plus gemcitabine for first-line treatment of Asian patients with advanced non-small-cell lung cancer harbouring EGFR mutations (LUX-Lung 6): an open-label, randomised phase 3 trial. Lancet Oncol. 2014; 15: 213-22.
13 Zhou C, Wu YL, Chen G, Feng J, Liu XQ, Wang C, et al. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): a multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011; 12: 735-42.
14 Soria JC, Ohe Y, Vansteenkiste J, Reungwetwattana T, Chewaskulyong B, Lee KH, et al. Osimertinib in Untreated EGFR-Mutated Advanced Non-Small-Cell Lung Cancer. N Engl J Med. 2018; 378: 113-25.
15 Sanchez de Cos Escuin J, Disdier Vicente C, Corral Penafiel J, Riesco Miranda JA, Sojo Gonzalez MA, Masa Jimenez JF. [Overall long-term survival in lung cancer analyzed in 610 unselected patients]. Arch Bronconeumol. 2004; 40: 268-74.
16 Fry WA, Phillips JL, Menck HR. Ten-year survey of lung cancer treatment and survival in hospitals in the United States: a national cancer data base report. Cancer. 1999; 86: 1867-76.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/