J Med Discov (2019); 4(3):jmd19020; DOI:10.24262/jmd.4.3.19020; Received June 24th, 2019, Revised July 22nd, 2019, Accepted August 06th, 2019, Published August 16th, 2019.
Imperforated hymen with transverse vaginal septum in a 15-year-old patient
Rasha A. Al-Lami1, Ammar M. A. Algburi2, Ihab Mahmood Hussein2
1University of Texas Medical Branch at Galveston, Department of Preventive medicine and Community Health, Texas, USA.
2Al-Yarmouk Teaching Hospital, Baghdad, Iraq.
* Correspondence: Rasha A. Al-Lami,University of Texas Medical Branch at Galveston, Department of Preventive medicine and Community Health, Texas, USA. Email: raallami@utmb.edu.
Abstract
Here we present a case of the imperforated hymen and transverse vaginal septum with associated hematometrocolpos, blood accumulation in the vaginal and uterine cavities, in a 15-year-old female patient. Virginity sparing technique was conducted given the cultural values of the patient and her family. The rarity of this condition along with special surgical technique in limited health care facility setting signifies this case report.
Keywords: obstructive reproductive tract; hymen; vaginal septum.
Introduction
Imperforated hymen is the most common cause of reproductive tract obstruction in female patients. It can occur with or without other associated anomalies like vaginal septum. The presentation of imperforated hymen is usually delayed until puberty when the patient will start to menstruate and accumulated blood in the vagina starts to exert mass effect on the surrounding structures with or without associated infection. The diagnosis can be made very early in infancy by visualizing the perineum for the presence or absence of hymeneal small opening. Ultrasound is the first imaging investigation to evaluate the presence of imperforate hymen and MRI is considered the best imaging technique to delineate the pelvic anatomy and associated urogenital anomalies. The management of imperforated hymen is almost always surgical with good future prognosis.
Case Report
A 15-year-old female patient who has not menstruated yet, presented to our unit with 3 months history of cyclic progressive lower abdominal pain and difficulty in urination that increased in intensity with time. The patient started to feel this pain during the past year but was repeatedly treated with antibiotics and pain killers for suspected urinary tract infection. On examination, menarche has not started yet. Patient weight was 47 kg (on 25th percentile for her age) and height was 145 cm (on 10th percentile for her age). Pubic hair, axillary hair and breast were Tanner stage 4. Pelvic examination revealed slightly protruding bluish hymen membrane, rest of the perineum was intact. On rectal examination, tender soft mass was palpated anteriorly to the rectum. Lab results in terms of renal and liver function tests as well as complete blood count and serum electrolytes were all normal. Imaging techniques in the form of Ultrasound and MRI as follows:
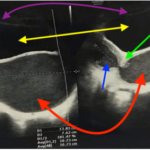
Pelvic U/S
Significantly distended vaginal canal occupied by large cystic lesion measured (13.8 * 7.6 cm) seen in continuity with another cystic lesion that extends into the uterine cavity. Endometrial cavity measures (4*2.2 cm) and contains fluid of intermediate echogenicity. Picture of hematocolpos and hematometra with imperforated hymen is most likely along with distended urinary bladder. No fluid in cul-de-sac, normal ovaries, normal bilateral kidneys and normal abdominal organs (Figure 1).
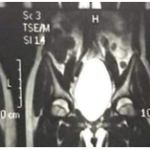
MRI of the pelvis
Uterus was markedly enlarged and distended with hemorrhagic fluid while the vaginal walls were normal and urinary bladder was filled and compressed anteriorly. No other lesion was detected (Figure 2).
Figure 1. Gynecologic-Pelvic Ultrasound showing the followings: • Red arrows: distended uterine cavity filled with fluid-hematometra. • Blue arrow: distended vaginal cavity filled with fluid-hematocolpos. • Green arrow: normal cervix. • Yellow arrows: distended urinary bladder. • Purple arrows: faint line delineating urinary bladder.
Surgical management
After obtaining parental consent, the patient was admitted to the surgical ward and was prepared to have surgical correction of imperforated hymen. The patient and her parents understood the complications and prognosis of the surgical technique. Patient and family emphasized the importance of sparing virginity during the procedure because of cultural values. Under general anesthesia in lithotomy position, bulging of thick blue appearing hymen was noticed. Small opening in the hymen was done to drain the accumulated old blood from the vaginal cavity. Obliteration of distal vagina was found for which dilatation of distal vagina was proceeded. Transverse vaginal septum occupying the lower third of the vaginal cavity was noticed. Slight dissection and suturing of the edge of the transverse vaginal septum to the edge of the hymen was done to increase the size of vaginal opening and minimize re-stenosis of distal vagina post-operatively. The cervix was dilated using Hegar dilator to evacuate hematometra. The induced hymeneal opening was sutured partially. During the procedure, injury to the urinary bladder was suspected upon which urology team was called. The urology team did cystoscopy that revealed posterior urethra and bladder neck injury. Required necessary urethral and urinary bladder repair was done with placement of suprapubic urinary catheter via cystostomy in addition to Foley’s catheter. The patient was given adequate antibiotics, suprapubic catheter was removed after 3 days and urinary Foley catheter was kept for 2 weeks. The patient was discharged from hospital after one week of admission. Hospital stay and post-operative period were uneventful. The patient was followed for 3 months period and started to expel menstrual blood normally with every 3 menses she had during the follow-up period. During each follow up visit the patient was examined for distal vaginal re-stenosis and counseled to schedule regular visits for evaluation. To this point, no vaginal re-stenosis has occurred nor any other complication related to the aforementioned surgical procedure like further injury to surrounding tissues. Also, patient did not develop new signs or symptoms to any known gynecological disease during follow-up time period.
Figure 2. Pelvic MRI with fat suppression technique (pre and post Intravenous contrast): Uterus markedly enlarged with hemorrhagic fluid (hematometra). Blue arrow: distended uterus, green arrow: compressed urinary bladder.
Discussion
The most widely accepted theory about normal embryological origin of the vagina suggested that the upper portion of the vagina was derived from the Mullerian duct while the lower part was a derivative of the urogenital sinus. In normal circumstances, female fetus external genitalia development begins around 4 weeks of gestational age and continues until around 12 weeks during which two structures can be identified between urethral and urogenital folds; the urogenital groove and membrane. Remnant of the latter will form the hymen after forming the two openings of urethra and vagina; thus, the hymen is embryologically derived from endoderm of urogenital sinus and failure of canalization of vaginal plate will lead to imperforated hymen with vaginal septum[1]. Transverse vaginal septum can present in upper third (46%), middle third (35%) or lower third of vagina (19%)[2]. Female obstructive reproductive tract anomalies’ genetic inheritance and over generation transmission have not been documented in human studies[1]. Imperforated hymen is considered the most common obstructive anomaly of female reproductive tract with incidence rate of 1 in every 70,000 live female births caused by urogenital sinus embryologic maldevelopment[2]. The most common presentation of imperforated hymen occurs during early adolescence in the form of primary amenorrhea associated with cyclic lower abdominal and pelvic pain. The accumulated blood inside the vagina, hematocolpos, can exert mass effect around surrounding structures causing constipation and urinary retention with possible future complication of infection, hydronephrosis and impairment of renal function.
Tumor marker CA-125 has been described in association with imperforated hymen presentation[3]. CA-125 is normally expressed in any tissue derived from coelomic epithelium such that of serosal surfaces, peritoneum, pericardium and pleura, as well as in Mullerian epithelium. The alarming association is the presence of carcinoma especially that of the ovary. In Kaya et al., they described a case of 15-year-old female with imperforated hymen with transverse vaginal septum presented with hematocolpos with elevated CA-125 of 80.2 U/ml (normal<30)[2].
Besides clinical history and examination, imperforated hymen diagnostic method of choice is magnetic resonance imaging (MRI). MRI is superior to CT scan in visualizing the pelvic anatomy and the extent of accumulated blood. MRI with contrast can provide information about mass consistency and capture the presence of vaginal septum or any other associated soft tissue anomaly; thus, MRI could serve as an asset in later guiding the management plan. MRI is non-invasive readily available technique than can be used safely in young patients. It can also exclude pelvic, renal, ovarian and uterine causes that carry similar clinical presentation as hematometrocolpos[3].
The standard management of imperforated hymen is by surgical hymenectomy with cruciate or X-like incision in the hymen; however, vaginal sparing techniques make this option hardly possible. Endoscopic techniques have been used to preserve virginity. The use of three-dimensional saline-solution contrast sonovagino- cervicography to guide transrectal ultrasound while endoscopic vaginoplasty is performed was preferable in treating imperforated hymen in cultures where virginity maintenance is socially important. In Egbe et al., X-shaped hemenectomy was performed with trimming of hymen leaflets to preserve some of its tissue to maintain virginity in their patient[4]. According to the latest American College of Obstetrics and Gynecology-ACOG- recommendations, simple incision and drainage of hematocolpos are not recommended by ACOG as it is highly associated with ascending infection to uterus. In the presence of transverse vaginal septum, distal vaginal atresia and cervical atresia, vaginal re-stenosis is a predicted complication after surgical correction; therefore, delaying the initiation of surgical correction, in order to get good amount of accumulated blood that would be helpful in functionally dilatating the distal vagina, is preferable to prevent future post-surgical re-stenosis. Prescription of oral medroxyprogesterone acetate- 20 mg orally three times/day, continuous combination of oral contraceptive pills or progesterone only pills can delay the menstrual cycle and ease the cyclical pain till surgical intervention initiated. However, the presence of urinary retention, severe pain or ascending infection mandate early surgical intervention. Long-term follow up is important to exclude the development of endometriosis, dysmenorrhea, infection and urinary and rectal injury. Also, 1-2 weeks hospital stay is recommended in addition to monthly visit thereafter[5].
Conclusion
In our case, MRI could not detect the lower vaginal septum. Owing to limited facility in our unit, small opening was done in the hymen followed by partial suturing. No re-stenosis was noticed in post-operative period. It is important to check for urinary bladder injury in similar surgical procedure and have the urology team involved. Although imperforated hymen is a rare condition, early intervention and treatment could save the patient from major adverse events like renal impairment. Standard surgical technique could not always be sought and carried given the available health care facilities and the cultural importance of virginity sparing.
Conflict of interest
None
Acknowledgments
Author discloses no acknowledgement. No funding was received for this case report.
References
1. Dietrich JE, Millar DM, Quint EH. Obstructive reproductive tract anomalies. J Pediatr Adolesc Gynecol. 2014;27(6):396-402.
2. Kaya C, Cengiz H, Ekin M, Yasar L. Transverse vaginal septum: a benign reason for elevated serum CA 19-9 and CA 125 levels. Archives of Gynecology and Obstetrics. 2012;286(3):821-823.
3. Kapsalaki E, Daponte A, Deligeoroglou E, Zavos A, Fezoulidis I, Messinis IE. The role of MRI in young adolescent girls with hematocolpos. European Journal of Radiology Extra. 2011; 78(2): e97-e100.
4. Thomas Obinchemti E, Fidelia Mbi K, Emmanuella Manka’a W. Virginity-sparing management of hematocolpos with imperforate hymen: case report and literature review. SAGE Open Medical Case Reports. 2019;7.
5. Management of Acute Obstructive Uterovaginal Anomalies: ACOG Committee Opinion, Number 779. Obstetrics & Gynecology. 2019;133(6).
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/