J Med Discov (2019); 4(3):jmd19016; DOI:10.24262/jmd.4.3.19016; Received May 24th, 2019, Revised June 18th, 2019, Accepted July 10th, 2019, Published August 8th, 2019
Ocular vestibular-evoked myogenic potentials, subjective visual vertical and subjective visual horizontal testing in patients with endolymphatic hydrops
Xiaomei Sun1, Yongkang Ou2, Yaodong Xu2,*
1Department of Otorhinolaryngology, Head and Neck Surgery, The sixth affiliated Hospital of SUN YAT-SEN University, Guangzhou, 510655, China
2Department of Otorhinolaryngology, Head and Neck Surgery, SUN YAT-SEN Memorial Hospital of SUN YAT-SEN University, Guangzhou, 510120, China
* Correspondence: Yao-dong Xu, Department of Otorhinolaryngology, Head and Neck Surgery, SUN YAT-SEN Memorial Hospital of SUN YAT-SEN University, Guangzhou, 510120, China. Tel: 86-020-81332580, E-mail: xuyaod@mail.sysu.edu.cn.
Abstract
Objective: To evaluate otolith function in patients with endolymphatic hydrops through ocular vestibular-evoked myogenic potentials (oVEMP), subjective visual vertical (SVV) and subjective visual horizontal (SVH) testing.
Methords: Fifty-one patients with endolymphatic hydrops, including Meniere’s disease (MD) and delayed endolymphatic hydrops (DEH), were included in the present study. All subjects underwent audiovestibular evaluation consisting of oVEMP, SVV, SVH and pure-tone audiometry and auditory brainstem response.
Results: 78.4% of patients showed abnormal oVEMP, 39.2% of patients had abnormal SVV, 49% of patients had abnormal SVH. The positive rate of SVV/SVH is 54.9%. The ratio of abnormal oVEMPs was higher compared to positive SVV/SVH ( P < 0.05).
Conclusion: Compared with SVV and SVH, oVEMP has a higher abnormality rate in MD and DEH patients. In terms of qualitative assessment of utricle function in patients, oVEMP has more sensibility than SVV/SVH. However, SVV/SVH is more valuable to evaluate whether the damage of the utricle function is compensated than the oVEMP.
Keywords: Ocular vestibular-evoked myogenic potentials (oVEMP); subjective visual vertical (SVV); subjective visual horizontal (SVH) ; endolymphatic hydrops
Introduction
Vertigo is a common otological symptom caused by many diseases. One of the most common pathological causes of repeated peripheral vertigo is endolymphatic hydrops, which includes Meniere’s disease (MD) and delayed endolymphatic hydrops (DEH).
During the last century, the physiological reflex pathway of the subjective visual vertical (SVV) and subjective visual horizontal (SVH) has been identified. The reflex originates from the utricle and appears to be bilaterally symmetrical for patients with peripheral vestibular disorders. Although subjective visual vertical (SVV) and subjective visual horizontal (SVH) tests can evaluate the utricle, it remains difficult to localize which side of the utricle lesions for patients with bilateral deficiencies. Ocular vestibular evoked myogenic potentials (oVEMP) have been proved to originate from the utricle[1, 2]. and it can be recorded on the surface by multiple acoustic stimuli[3-8]. The blink reflex does not affect these potentials[9, 10]. Animal experiments and clinical electrophysiological experiments have confirmed that the oVEMP, SVV and SVH are generated by the utricle via the upper vestibular nerve pathway. However, there is no literature reported about the relationship among oVEMP, SVV and SVH in the MD and DEH patients. What are the characteristics of the three clinical manifestations of the utricle and upper vestibular nerve conduction pathway in patients with endolymphatic hydrops? What is the relationship between these three clinical testing methods?
Materials and Methods
Fifty-one patients who were clinically diagnosed as endolymphatic hydrops were recruited at SUN YAT-SEN Memorial Hospital, SUN YAT-SEN University during 2012.8 ~ 2013.4. All the patients are during an acute attack. And all patients can cooperate with all of the examinations. The study was approved by the ethical review board of Sun Yat-sen Memorial Hospital, Sun Yat-sen University, China, and informed consent was obtained from all participants. Clinical Data Collection
All patients had their medical records examined in detail and underwent specialized physical and laboratory examination to confirm the diagnosis. Detailed medical records including age, gender, and duration of the disease, laterality, symptoms, other pertinent details. Physical exam including the Romberg test, M-ann test, Babinski-Weil walking test. Audiological tests included pure tone audiometry, auditory brainstem response, electro- cochleogram vestibular function tests included oVEMP, SVV, SVH, cVEMP,caloric test and head shake test. Computed tomography or magnetic resonance imaging were selectively conducted
SVV and SVH tests use the French (Synapsys) vertical subject1.3.2.66 for testing. Patients sit up and hold their head in erect and middle in a darkroom. Patients wear eye masks to eliminate visual reference. Tests set visual background into black and target into white light projections; cursor distance set to 2m, length is 60cm, the range of initial position is within ±25°. Testers use a remote control within ±0.1° accuracy to adjust cursor angle. After two unrecorded practice trials, subjects put on their eye masks to begin recorded testing. The mean of three SVV and SVH trials was calculated. During the test, SVV is in the zero degree position when centered. Rightward deflection is recorded as “+” and leftward deflection is recorded as “-”; SVH is in the zero degree position when in the horizontal plane. Upward deflection is recorded as “+” and downward deflection is recorded as “-”. The result of SVV and SVH tests tilting angles will be recorded as absolute values for convenient calculation.
The tilting angles between -2.00° and 2.00° are defined as normal, others beyond the range are defined as abnormal results marking as positive[11, 12].
During the IHS evoked potential system test, people lay flat in an anechoic chamber and locked vision on a target within 25-30 degrees of midline. In order to maintain inferior oblique muscle tension, people refrained from blinking and relaxed palatine muscles. Recording electrodes ere set 1 cm below the centre of the lower eyelid and reference electrodes were positioned about 2cm below the recording electrodes. Both recording electrodes and reference electrodes were in line with the ipsilateral pupil. Grounding electrodes were placed on the forehead between the eyebrows; this is referred to as the Fz point. The skin was cleaned before electrode placement and interelectrode resistance was kept less than 5 kΩ. By setting a window length of 50 ms, the apparatus applied a 500 Hz tone burst stimulus with an intensity of 100 dB HL. The signal intensity increased by 10,000 times and the super position on average increased by 128 times.
Parameter recording: the apparatus sent sound to one ear and recorded the oVEMP wave response from the contralateral orbit. The oVEMP latency period lasts from the beginning of the test to the duration of N1 peak to P1 peak (ms); the wave interval is the duration from N1 peak to P1 peak (ms); the amplitude is the vertical distance from N1 peak to P1 peak (uv).The oVEMP waveforms which appear as waveform missing, decreased or increase of the amplitudes in the diseased ear is defined abnormal.
SPSS 19.0 software is adapted to statistical analysis in this study. Comparison between groups were performed by McNemar test, and p< 0.05 was considered statistically significant.
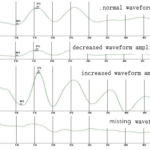
Fig. 1 oVEMP waveforms of the patients
Results
In this study, 51 patients aged from 18 to 69 ( 43.86±14.01). Twenty-eight patients were males and twenty-three patients were females. There are 42 patients with MD and 9 patients with DEH.
In terms of oVEMP. 78.4% (40/51) of the patients had abnormal oVEMP tests. 21.6% (11/51) had normal wave characteristics. 13.7% (7/51) of the patients had decreased amplitudes in diseased ear amplitudes. 3.9% (2/51) of patients had increased amplitudes in diseased ear amplitudes. 35.3% (18/51) of patients had missing waveform in the diseased ear. 25.5% (13/51) of patients had missing waveform for both ears. (Table 1) (Figure 1)
Fifty-one subjects completed SVV and SVH test. SVV tilt angles distributions for patient are shown in Figure 2A, Figure 2B. 61% (31/51) of patients had SVV tilting angles between -2゚and +2゚. And 39% (20/51) of patients showed SVV tilting angles beyond it. 51% (26/51) of patients had SVV tilting angles between -2゚ and +2゚. And 49% (25/51) of patients showed SVH tilting angles beyond it. The tilting angles between -2.00° and 2.00° are defined as negative, others beyond the range are defined as positive. Correlation analysis of SVV and SVH shows that there is a correlation between the two. (p < 0.001, r = 0.578) (Table 2).
Table. 1 the oVEMP test results of patients
| oVEMP | Normal | Amplitude reduction for diseased ear | Amplitude increase for diseased ear | Missing wave for diseased ear | Missing wave for bilateral ear | Total |
| Case number | 11 | 7 | 2 | 18 | 13 | 51 |
| Percentage of cases | 21.6% | 13.7% | 3.9% | 35.3% | 25.5% | 100% |
Table 2 SVV and SVH positive frequency in patient (n=51).
| SVH | Analysis | ||||
| Negative | Positive | p | r | ||
| SVV | Negative | 23 | 8 | 0.001* | 0.578 |
| Positive | 3 | 17 | |||
*p<0.001
Fig. 2 (A) The SVV tilting angle in patients. (B) The SVH tilting angle in patients
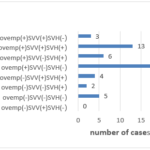
The results of the SVV, SVH, oVEMP in the patiens showed multiple. 13 patients showed all of the tests abnormal, and 5 patients showed all of the test normal. The rest patients showed abnormal at least one of the three tests. figure 3.
78.4% of patients showed abnormal oVEMP, 39.2% of patients showed abnormal result in SVV, 49% of patients showed abnormal result in SVH. We defined any test result of abnormal SVV or abnormal SVH as the SVV/SVH positive. The positive rate of SVV/SVH is 54.9%. The frequency of abnormal oVEMPs compared to positive SVV/SVH showed statistical significance; p <0.05. The frequency of abnormal oVEMP was greater than the frequency SVV/SVH (Table 3).
Table. 3 comparison between the result of SVV/SVH and oVEMP in the patients (n=51)
| oVEMP | |||
| Negative | Positive | ||
| SVH/SVH | Negative | 5 | 18 |
| Positive | 6 | 22 | |
| p | 0.023 | ||
*p<0.05
Fig.3 The three tests results of the patients
Discussion
Lopez[13] and others found the brain’s neuronal network has an effective and constantly updating internal model for sensing vertical direction whose primary purpose is postural stability and movement control. However, tests for vestibular otolithic function have much inter-laboratory variability, including cursor length, initial cursor position and the distance between the cursor and subject.
Animal experiments and clinical electrophysiology experiments confirm that SVV and SVH reflexes through the vestibulo-ocular reflex pathway result in eye torsion that manifest as SVV and SVH deviation. For patients with peripheral vestibular damage, their bilateral utricle function are with poor symmetry. oVEMP through vestibulo-ocular reflection change results in absent or abnormal extraocular muscle electromyography, and the reaction stimulates utricle function. Schonfeld[14] and others performed SVV, cVEMP and caloric tests on 538 patients with decreased unilateral peripheral vestibular function. The abnormal rate was 74%. However, SVV abnormality rate was only 30%. Patients with abnormal SVV mainly showed postural instability and unstable motor function.
In our experiments, the oVEMP abnormality rate in patients with MD and DEH was 78.4%, SVV abnormality rate was 39.2% and SVH abnormality rate was 49%. Abnormality rates comparisons between oVEMP and SVV and between oVEMP and SVH showed statistical significance. The oVEMP abnormality rate is significantly greater than those of SVV and SVH, showing a common response to utricle to superior vestibular nerve pathway integrity and showing that oVEMP has higher sensitivity than SVV and SVH in assessing this pathway’s integrity. Helling[15] found that 18% of patients that had normal SVV tests had abnormal test results when further testing with coaxial rotation was applied. The possibility of false negative test results further reduces the sensitivity of SVV and SVH.
Some patients in our experiments showed normal SVV and SVH, but had abnormal oVEMP. There are two possible explanations. SVV and SVH may have a false negative. Rotary and static SVV and SVH tests combined may increase test sensitivity. Another possible explanation is that patients with MD and DEH were during repeated attacks. Attack duration ranges from 10 to 15 days. Their history of recurrent attacks of acute vertigo may reflect multiple insults to utricle function. Reversible and irreversible damage to the utricle may cause reduced sensitivity to sound stimulation. This is the primary reason for abnormal or non-elicited oVEMP waves. After unilateral utricle function damage, adjustments from visual signal inputs increase in function and compensate[16]. Vertigo patients with proper compensatory adjustment may have normal SVV and SVH, but have non-elicited oVEMP.
Combining physiopathologic basis of oVEMP, SVV and SVH, we believe that the functional status of the utricle and whether hydrops lesions affect the utricle can be evaluated by oVEMP combined with SVV and SVH tests when patients with MD and DEH were during vertigo attacks. Dynamic multiple checks of SVV and SVH tests on patients with acute MD and DEH can track the dynamic compensation process after unilateral damage. Therefore, oVEMP combined with SVV and SVH tests can evaluate the state of damage of the utricle – superior vestibular nerve pathway and the compensation after vertigo attack. According to our study, we infer that patients with peripheral vertigo showing normal SVV, SVH, and oVEMP measurements indicate that the utricle is not affected. However, patients with normal SVV and SVH but abnormal oVEMP indicate that the utricle is damaged but has been compensated.
Conclusion
Compared with SVV and SVH, oVEMP has a higher abnormality rate in MD and DEH patients. In terms of qualitative assessment of utricle function in patients, oVEMP has more sensibility than the SVV/SVH. However, SVV/SVH is more valuable to evaluate whether the damage of the utricle function is compensated than the oVEMP.
Conflict of interest
None
Acknowledgments
None
References
1. Curthoys, I.S. (2012) The interpretation of clinical tests of peripheral vestibular function. Laryngoscope 122 (6), 1342-52.
2. Taylor, R.L. et al. (2012) Vestibular evoked myogenic potentials to sound and vibration: characteristics in vestibular migraine that enable separation from Meniere’s disease. Cephalalgia 32 (3), 213-25.
3. Chihara, Y. et al. (2009) Ocular vestibular-evoked myogenic potentials (oVEMPs) require extraocular muscles but not facial or cochlear nerve activity. Clin Neurophysiol 120 (3), 581-7.
4. Curthoys, I.S. et al. (2011) The ocular vestibular-evoked myogenic potential to air-conducted sound; probable superior vestibular nerve origin. Clin Neurophysiol 122 (3), 611-616.
5. Park, H.J. et al. (2010) Frequency-tuning characteristics of cervical and ocular vestibular evoked myogenic potentials induced by air-conducted tone bursts. Clin Neurophysiol 121 (1), 85-9.
6. Walther, L.E. et al. (2011) [Air conducted ocular VEMP: I. Determination of a method and application in normal patients]. Laryngorhinootologie 90 (7), 410-5.
7. Wang, S.J. et al. (2010) Ocular and cervical vestibular-evoked myogenic potentials: a study to determine whether air- or bone-conducted stimuli are optimal. Ear Hear 31 (2), 283-8.
8. Chihara, Y. et al. (2007) Vestibular-evoked extraocular potentials by air-conducted sound: another clinical test for vestibular function. Clin Neurophysiol 118 (12), 2745-51.
9. Smulders, Y.E. et al. (2009) The n10 component of the ocular vestibular-evoked myogenic potential (oVEMP) is distinct from the R1 component of the blink reflex. Clin Neurophysiol 120 (8), 1567-76.
10. Iwasaki, S. et al. (2007) Head taps evoke a crossed vestibulo-ocular reflex. Neurology 68 (15), 1227-9.
11. Davalos-Bichara, M. and Agrawal, Y. (2014) Normative results of healthy older adults on standard clinical vestibular tests. Otol Neurotol 35 (2), 297-300.
12. Hirvonen, T.P. et al. (2011) Subjective head vertical test reveals subtle head tilt in unilateral peripheral vestibular loss. Eur Arch Otorhinolaryngol 268 (10), 1523-6.
13. Lopez, C. et al. (2011) Spatiotemporal dynamics of visual vertical judgments: early and late brain mechanisms as revealed by high-density electrical neuroimaging. Neuroscience 181, 134-49.
14. Schonfeld, U. et al. (2010) Evidence of unilateral isolated utricular hypofunction. Acta Otolaryngol 130 (6), 702-7.
15. Helling, K. et al. (2006) Testing utricular function by means of on-axis rotation. Acta Otolaryngol 126 (6), 587-93.
16. Lord, S.R. and Webster, I.W. (1990) Visual field dependence in elderly fallers and non-fallers. Int J Aging Hum Dev 31 (4), 267-77.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/