J Med Discov (2019); 4(1):jmd18041; DOI:10.24262/jmd.4.1.18041; Received October 06th, 2018, Revised January 19th, 2019, Accepted February 13rd, 2019, Published March 01st, 2019
Renal Dysfunction & Its Association With BNP, NT-pro BNP: A Case Report
Mohammad Ali Raza Qizalbash1, *, Rida Zahra2, Younus Dheyaa Al-Midfai3, David Peter Uhlenberg4
1Department of Internal Medicine, Dalian Medical University, Dalian, China.dr_aq@hotmail.com
2Medical student, University College of Medicine & Dentistry, Lahore, Pakistan. dr_ridazahra@hotmail.com
3Department of Internal Medicine, Al-Furat general hospital, Baghdad, Iraq. dr.ydy@yahoo.com
4Department of Internal Medicine, University of Pecs, Hungary. unlenbergdavid@gmail.com
* Correspondence: Mohammad Ali Raza Qizalbash, M.D. Lahore, Pakistan. Tel: +92 3123121470. E-mail: dr_aq@hotmail.com.
Abstract
Background: Cardiac natriuretic peptides are associated with cardiac injury. B-type natriuretic peptide (BNP) and amino-terminal pro-B-type natriuretic peptide (NT-proBNP) are biomarkers of cardiovascular disease that is common in patients with chronic kidney disease (CKD). Patients with chronic kidney disease (CKD) are at increased risk of cardiovascular disease. Natriuretic peptides (NPs), biomarkers of myocardial dysfunction, offer the potential for early detection and risk stratification of cardiac disease. This screening utility could be extended to CKD patients asymptomatic of cardiovascular disease.
Case Presentation: A male 49 years old with chronic renal failure for 10 years presented for follow up and we find increase level of BNP and NT-proBNP levels.
Conclusion: Measuring BNP and NT-proBNP levels in patients with Chronic Kidney disease can help physicians to screen for cardiac dysfunction in CKD.
Keywords: Chronic Renal Failure, Heart Failure, Cardiac Natriuretic Peptides.
Introduction
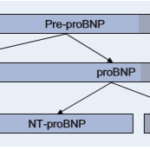
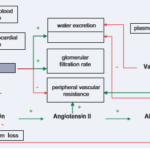
Natriuretic peptides are a family of vasoactive peptides which are involved in the control of water and sodium homeostasis (Figure 1 and 2). They are thus part of a regulatory system that is commonly activated in cardiac as well as renal failure. Formerly the B-type natriuretic peptides BNP and NT-proBNP in particular gained importance as reliable markers for diagnosis and risk stratification in heart failure patients. More recently it has been shown that the plasma concentrations of these cardiac neurohormones are also increasingly elevated in patients with progressively impaired renal function. Nevertheless, the natriuretic peptides were also found to be of diagnostic and prognostic value in this group of patients, who are at enormously elevated risk of cardiovascular disease, though with higher cutoffs. In addition, most recent data indicate that high BNP or NT-proBNP levels are associated with accelerated progression of chronic kidney disease. B-type natriuretic peptides may therefore evolve as markers of the cardiorenal syndrome. The most common cause of death in patients with Chronic Kidney Disease is Heart Failure1.
Fig. 1 Biosynthetic pathway of human BNP
Fig. 2 Physiological action of BNP
Case presentation
A Caucasian male 49 years old with a Hx of stage 3 Chronic Kidney disease for 10 yrs. presented for regular follow up to our outpatient clinic. This is his second visit in 9 months. Patient complaints of low energy level, weakness, muscle cramps and bilateral lower limbs edema.
The patient denies palpitation, dyspnea, orthopnea, Paroxysmal nocturnal dyspnea, hematuria, dysuria, urgency, nocturia, joints pain, and weight changes. Past medical history is significant for hyperlipidemia for 7 years for which he is taking statins. No other medical or surgical history. No significant family history, no allergy, smoking, alcohol or drug abuse.
Patient’s vital signs: Blood pressure 121/83 mmhg, pulse 73 b/min and respiration 14/min and temperature 98.8°f.
General physical examination was normal except for bilateral +2 pedal edema.
Heart/Chest examination: normal auscultation, peak maximal impulse (PMI) non-displaced, no carotid bruit, normal jugular venous pressure (JVD) and respiratory sounds were normal.
Abdominal examination was normal with no ascites, no costovertebral angle tenderness or flank mass.
Blood test and Renal Function test
| Blood test | results |
| Creatinine | 2.3 mg/dl |
| BUN | 66 mg/dl |
| Sodium | 138 mmol/L |
| Potassium | 5.3 mmol/L |
| Calcium | 8.9 mg/dl |
| Chloride | 105 mmol/L |
| Bicarbonate | 21 mmol/L |
|
Phosphorous WBC Hb Platelet |
4.6 mg/dl 8.2 x 109/L 12 g/dl 263×109/L |
Table 1. Metabolic profile.
Cardiac peptides at presentation and after 9 months
| BNP | NT-Probnp | |
| At presentation | 48pg/ml | 98 pg/ml |
| After 9 months | 56pg/ml | 161 pg/ml |
Table 2. Cardiac Natriuretic Peptides.
Serologies
Negative hepatitis and HIV serology.
Negative antinuclear antibody (ANA), classical antineutrophil cytoplasmic antibody (c-ANCA), Protoplasmic-Staining antineutrophil cytoplasmic antibody (p-ANCA).
Lipid test
Total cholesterol 357 mg/dl, Triglyceride 313 mg/dl, HDL 34 mg/dl, LDL 260 mg/dl.
Urine analysis
1-3 RBCs, 0-2 WBCs and 24-hour albumin to creatinine ration (ACR) = 21.3mg/mmol. Glomerular Filtration Rate (GFR) = 51 mL/min/1.73 m2 in (80 kg male).
Classification of GFR
CKD is classified as stage 3 based on NKF/DOQI guidelines.
Reference range > 60 ml/min/1.73m2.
| Stage | Comment |
| Stage 1 or 2 | normal or mild decrease in renal function. |
|
Stage 3 Stage 4 Stage 5 |
moderate decrease in renal function. severely reduced renal function. very sever or end stage renal failure.
|
Table 3. Classification of GFR.
On the basis of history, physical exam, and laboratory evidence patient was diagnosed with Chronic Kidney Disease Stage 3.
Transthoracic Cardiac ECHO finding at presentation and after 9 months
| At presentation |
Champers dimensions: No evidence of hypertrophy is noted or dilation in cardiac champers, no evidence of intracardiac thrombus or pericardial effusion is identified. No septal defect is seen.
Ventricular function: The global ejection fraction is calculated at 55% +/- 4% with no focal wall motion abnormalities.
Valves: Mild mitral valve regurgitation.
|
| After 9 months |
Champers dimensions: No evidence of hypertrophy is noted or dilation in cardiac champers, no evidence of intracardiac thrombus or pericardial effusion is identified. No septal defect is seen.
Ventricular function: The global ejection fraction is calculated at 53%. This is within normal limit.
Valves: Mild mitral valve regurgitation.
|
Table 4. Transthoracic Echocardiography.
Renal Ultrasound
No hydronephrosis, renal stone or mass.
Reduced renal length.
Normal renal cortical echogenicity and thickness.
Poor visibility of the renal pyramids and the renal sinus.
No renal artery stenosis and patent renal veins.
Discussion
BNP and NT-proBNP were introduced as biomarkers for heart failure but have also found useful as markers for mortality in acute coronary syndromes and myocardial infarction.2 Renal dysfunction or failure represents a variable that complicates the interpretation of these markers.
As with acute heart failure evaluation, knowledge of the cardiac and noncardiac factors that influence BNP and NT-proBNP concentrations is necessary. Natriuretic peptides have a principal effect on the kidney promoting tubular natriuresis and diuresis. Falls in cardiac output, effective blood volume, and renal blood flow are accompanied by activation of the renin-angiotensin-aldosterone system and sympathetic nervous system. BNP action opposes the effects of the renin-angiotensin-aldosterone system, promoting natriuresis and increasing GFR.3 In simpler terms, increased intravascular volume, resulting from heart failure or renal dysfunction, increases the secretion of BNP; BNP acts through the kidney to reduce intravascular volume, thereby decreasing the stimulus for BNP secretion. Renal dysfunction decreases this effect, requiring more BNP to achieve the same level of activity in the normal kidney. Heart failure decreases the effectiveness of the kidney, simulating renal dysfunction. Thus, heart failure and renal dysfunction act synergistically in their ability to increase the secretion rates of BNP and NT-proBNP. In addition, decreased renal function reduces the clearance of BNP and NT-proBNP.
Takami et al4 found that patients with renal impairment had a greater level of serum BNP than patients with hypertension and normal renal function. These Cardiac Natriuretic Peptides can be used in patients with Chronic Kidney disease to help physicians to screen for cardiac dysfunction in CKD.
In summary, the recent publication by van Kimmenade et al. (6) and the study by Niizuma et al. (5) provide possible mechanisms to explain increased BNP and NT-proBNP concentrations seen in prior association and prognostic studies in patients with moderately impaired renal function (5)(6). Taken together, they indicate that increased BNP and NT-proBNP concentrations are predominantly related to and a result of the presence and extent of cardiac pathology rather than impaired renal clearance.
Conclusion
It is intriguing to postulate that in CKD patients with elevated plasma levels of BNP or NT-proBNP therapeutic interventions aimed at improving cardiac function could slow down the progression of CKD. Intervention studies, which are needed to underpin this concept, could also provide evidence for the causal relationship between cardiac malfunction, increased B-type natriuretic peptide concentrations and CKD progression.
Conflict of interest
None
Acknowledgments
All authors contributed equally. No funding grant was taken to write this article.
Ethical Approval
Informed consent was taken from the patient for publication of this case report.
References
1 Pornpen srisawasdi, Somlak Vanavanan et al. The Effect of Renal Dysfunction on BNP, NT-proBNP, and Their Ratio. American Journal of Clinical Pathology. 2010; 133:14-23.
2 Omland T Persson A Ng L et al. N-terminal pro B-type natriuretic peptide and long-term mortality in acute coronary syndromes. Circulation. 2002; 106:2913–2918.
3 Holmes SJ Espiner EA Richards AM et al. Renal endocrine and hemodynamic effects of human brain natriuretic peptide in normal man. J Clin Endocrinol Metab. 1993; 76:91–96.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/