J Med Discov (2018); 3(4):jmd18044; DOI:10.24262/jmd.3.4.18044; Received November 13rd, 2018, Revised December 03rd,2018, Accepted December 06th, 2018, Published December 12nd, 2018
Childhood Hepatoblastoma in two year old male- A case report
Sally Hannoodee1, Ahmed Z. Zain2,*
1Alnahrain university college of medicine.M.D., Baghdad/Iraq.
2Cosultant pediatric surgery,associated Professor- Alnahrain university, College of medicine-FIBMS pediatric surgery, Baghdad/Iraq.
* Correspondence: Ahmed Z. Zain , M.D. F.I.B.M.S. Pediatric surgery, Baghdad/Iraq. E-mail: drsallytalal@gmail.com
Abstract
Hepatoblastoma (HB) overall is a very rare tumor that affects the liver in infancy and childhood, it is the most common primary malignant tumor of the liver in that age . We reported a case of a 2-year old male child presented with pallor, abdominal distention; in physical examination there was a palpable large painless abdominal mass. CT scan reveled a solid hepatic tumor. His complete blood count shows thrombocytosis. Serum alpha feto- protein level was raised. A hepatic tumor in a child under the age of 3 years, associated with thrombocytosis and elevated serum alpha feto protein is very likely to be hepatoblastoma. The mainstay of treatment for this patient is surgical removal of the mass and then chemotherapy.
Keywords: Hepatoblastoma (HB); Abdominal mass; Thrombocytosis; Alpha feto protein(AFP); Child
Introduction
During 2002–2008 the rate of HB in the United States Surveillance, Epidemiology and End Results (SEER) program data were 10.5 and 5.2 cases per million children <1 and 1–4 years, respectively, and was too infrequent thereafter to calculate incidence. An estimate of SEER data in 1999 suggested that about 100 cases of HB are diagnosed each year in the United States. However, as incidence of HB has risen roughly 4% per year between 1992 and 2004, faster than for any other childhood cancer, the current number of cases per year likely is higher(1) so Hepatoblastoma is a very rare cancerous tumor that starts in the liver yet it is the most common primary malignant hepatic tumor of infancy and childhood, occurring predominantly in the first three years of life(2).
This tumor accounting for just over 1% of pediatric cancers. The etiology is unknown; the pathogenetic mechanisms responsible for the development of HB remain unclear. HB, as an embryonal tumor, is derived from undifferentiated embryonal tissue. Rapidly growing HBs often are very sensitive to cytotoxic drugs and sometimes are very sensitive to radiotherapy. HB has been associated with Beckwith-Weidemann syndrome, familial adenomatosis polypi, and low birth weight(3). The primary treatment is surgical resection; neoadjuvant chemotherapy particularly in unresectable tumors resulting in considerable preoperative tumor shrinkage and sometimes near total ablation of the tumor(4). Formerly a disease with a dreadful prognosis, children now have a 5-year survival rate of over 70%. This has been achieved by advances in surgical techniques and the use of chemotherapy(5).
Case Report
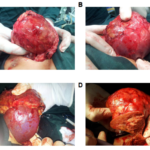
A 2-year-old male patient presented with 1 month history of enlarging abdomen, noticed by the mother while bathing him. Initially painless, now complains of dull aching pain and occasional vomiting unrelated to food intake. There was no past medical history of jaundice, anorexia and the patient was up to date with his vaccination schedule. His temperature was 37.2 C (98.96 F), blood pressure was 90/50 mm Hg, pulse was 110/min and regular, and respirations were 30/min. His weight was 11kg(75 percentile) and the height was 83 cm(90 percentile). On general examination, patient was having good general status, pallor and anemia. On abdominal examination, the liver was palpable about 6cm below the costal margin (figure 1) and spleen was just palpable. Hematological investigation revealed moderate anemia (Hemoglobin-8g/dl; Hematocrit-28%), thrombocytosis (platelets-850,000/mm3), normal liver function tests (ALT 13 Iu/I, AST 38Iu/I). USG abdomen suggested well defined mass noted in right lobe of the liver with the possibility of Hepatoblastoma. Further investigation in the form of CT scan (figure 2) confirmed the diagnosis of Hepatoblastoma affection the right lobe of the liver. Serum Alpha Feto Protein(AFP) was high: >1000 ng/ml(normal values <20 ng/ml). Hepatitis B and C and HIV tests were negative. The patient’s age, clinical data, high value of AFP and thrombocytosis raised the suspicion of a hepatoblastoma. However, the final diagnosis relied on the microscopic examination of the tumor biopsy therefore USG guided liver biopsy was taken. The microscopic examination of the liver biopsy showed cells arranged in solid sheets and trabecular pattern. The cells had distinct cell membrane, uniform nuclei with minimal pleomorphism. There was presence of fetal pattern and foci showing rosset formation and tabeculae, having poorly defined cell borders and basophilic cytoplasm suggestive of embryonal pattern. Overall features were consistent with clinical diagnosis of Hepatoblastoma. For this patient we did a Complete resection of the tumor (figure 3).
Figure 1: Abdominal examination of the patient demonstrate the large mass of the liver that can be palpated
Figure 2: Abdominal computed tomography revealed the mass of the liver.
Figure 3 Intraoperative image represent the large liver tumor from our patient. A. represent the tumor (size 8.5cm x 10cm). B. represent the tumor (size 8.5cm x 10cm). C. represent the tumor attachment to the healthy liver(the tumor before the surgical resection). D. represent the beginning of the resection of the tumor after determining the margin of the tumor.
Discussion
The most common primary malignant liver neoplasm in children is hepatoblastoma(6). The median age of onset of hepatoblastoma is approximately 16 months with a slight male predominance.The triad of a hepatic tumor, thrombocytosis and high level of serum AFP in a child between 6 months and 3 years age is diagnostic of hepatoblastoma(7).
Serum level of Alpha Feto Protein(AFP) should be interpreted according to age, high values indicating hepatoblastoma . Moderately high values of blood serum fetoprotein are often detected in types of hepatoblastoma, tumor of yolk sac, hepatocarcinoma as well as in certain benign tumors (mesenchymal hamartoma, focal nodular hyperplasia and infantile hemangioendothelioma)(8).
The hepatoblastoma diagnosis is established according to clinical (young age), imaging, serum (very high AFP serum level) and histological criteria. Thrombocytosis, frequently seen in children with hepatoblastoma and other malignancies, is considered a paraneoplasic phenomenon. Thrombocytosis usually seen because of the excessive production of thrombopoietin at the level of the tumoral tissue. The human thrombopoietin, also called growth factor of the megakaryocytes, is secreted by hepatocytes, kidneys, spleen and stromal cells of the bone marrow. The level of the serum thrombopoietin stimulates the megakaryocytopoiesis and determines the increase of the thrombocytes number(9-11) . Immunohistochemistry for hepatocyte antigen, alpha fetoprotein, and, in some instances, ß-catenin may be useful in the diagnosis of hepatoblastoma, mostly for tumors with favorable and unfavorable histologies. There is no immunostain to differentiate hepatocellular carcinoma from hepatoblastoma. Possible genetic markers (trisomies for chromosomes 2 , 20 and 8, abnormalities of chromosome 1p) may help differentiate these two entities, but only in approximately 35% to 40% of hepatoblastomas that carry the abnormalities(12).
The imaging work-up used at our institution begins with spiral CT for initial staging of the tumor and for assessing its resectability. It is also used to monitor tumor response to preoperative chemotherapy and search for tumor recurrence.
only complete surgical excision (as in our patient ) of the primary tumor was felt to correlate with cure. Complete resection of the tumor remains the best hope for long-term survival; however, the advent of effective chemotherapy may permit cure in the presence of initially unresectable or metastatic disease. If at initial surgical laparotomy the neoplasm seems resectable, safe attempt should be made to remove the tumor. If the tumor is deemed unresectable and the patient is at high risk for complications, a biopsy is taken and pre-resection chemotherapy is indicated(13-14).
Hepatoblastoma is taken into account to be non-surgical when: the tumour is extraordinarily giant, involving the danger of severe hemorrhage; both hepatic lobes are altered; the hepatic vein or the inferior vena cava is affected. The hepatic transplant is indicated either initially, for the non-excisable hepatoblastoma or after the relapse(15). Multicentric studies demonstrated a 10-year survival of 85 % in the case of children with a primary hepatic transplant and of 40 % in the case of those who needed a hepatic transplant after the relapse(16).
The AFP level monitoring represents a valuable marker of the response to the pre-surgical chemotherapy, in the evaluation of the excision result and for the precocious diagnosis of the hepatoblastoma relapse (17).
Conclusion
Hepatoblastoma(HB) is the most common malignant primary liver tumor in children. The primary treatment is surgical resection, and the use of pre-resection chemotherapy can increase the number of tumors that are resectable. The prognosis for patients with resectable tumor is fairly good in combination with chemotherapy. The outcome for those with non-resectable or recurrent disease remains poor.
Conflict of interest
None
Acknowledgments
None
References
1. Spector L. and Birch J. The epidemiology of Hepatoblastoma. Pediatr Blood Cancer. 2012 Nov;59(5):776-9.
2. Sharma D, Subbarao G and Saxena R. Hepatoblastoma. Semin Diagn Pathol. 2017 Mar;34(2):192-200.
3. Herzog C, Andrassy R, and Eftekhari F. Childhood Cancer: Hepatoblastoma. The Oncologist 2000; 5:445-453.
4. Andrassy RJ, Brennan LP, Siegel MM et al. Preoperative chemotherapy for hepatoblastoma in children: report of six cases. J Pediatr Surg 1980;15:517-522.
5. Roebuck D and Perilongo G. Hepatoblastoma: an Oncological review. Pediatr Radiol (2006) 36: 183–186
6. Raney B. Hepatoblastoma in children: A review. J Pediatr Hematol Oncol. 1997 Sep-Oct;19(5):418-22.
7 Perilongo G, Shafford EA. Liver tumors. Eur J Cancer 1999; 35: 953- 959.
8. Schnater JM, Kohler SE, Lamers WH, von Schweinitz D, Aronson DC. Where do we stand with hepatoblastoma? A review. Cancer 2003; 98: 668-678
9. Shafford EA, Pritchard J. Extreme thrombocytosis as a diagnostic clue to hepatoblastoma. Arch Dis Child 1993; 69: 171.
10. Komura E, Matsumura T, Kato T, Tahara T, Tsunoda Y, Sawada T. Thrombopoietin in patients with hepatoblastoma. Stem cells 1998; 16: 329-333.
11. Hwang SJ, Luo JC, Li CP, et al. Thrombocytosis: a paraneoplastic syndrome in patients with hepatocellular carcinoma. World J Gastroenterol 2004; 10: 2472-2477.
12. Finegold MJ. Hepatic tumors in childhood. In: Russo P, Ruchelli ED, Piccoli D, eds. Pathology of Pediatric Gastrointestinal and Liver Dis ase. New York, NY: Springer-Verlag, 2004; 300-346.
13. Andrassy RJ, Brennan LP, Siegel MM et al. Preoperative chemotherapy for hepatoblastoma in children: report of six cases. J Pediatr Surg 1980;15:517-522.
14. Pierro A, Langevin AM, Filler RM et al. Preoperative chemotherapy in “unresectable” hepatoblastoma. J Pediatr Surg 1989;24:24-28.
15. Czauderna P, Otte JB, Aronson DC, et al. Guidelines for surgical treatment of hepatoblastoma in the modern era-recommendation from the childhood Liver Tumour strategy Group of International Society of Pediatric Oncology (SIOPEL). Eur J Cancer 2005; 41:1031-1036.
16. Otte JB, Pritchard J, Aronson DC, et al; International Society of Pediatric Oncology (SIOP). Liver transplantation for hepatoblastoma: results from the International Society of Pediatric Oncology (SIOP) study SIOPEL-1 and review of the world experience. Pediatric Blood Cancer 2004; 42: 74-83.
17. Kubota M, Yagi M, Kanada S, et al. Effect of postoperative chemotherapy on the serum alpha-fetoprotein level in hepatoblastoma. J Pediatr Surg 2004; 39:1775-1778.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/