J Med Discov (2018); 3(4):jmd18031; DOI:10.24262/jmd.3.4.180301; Received July 14th, 2018, Revised September 20th, 2018,Accepted October 25th, 2018, Published November 28th, 2018.
Extra Pulmonary Tuberculosis: A Review on Current Scenario
Supriya Sharma1, Jyoti Bajpai2, Kanchan Srivastava2, Priyanka Gaur3, Surya Kant4*
1Department of Oral Pathology and Microbiology, Faculty of Dental Sciences, King George’s Medical University (KGMU), UP, Lucknow.
2Department of Respiratory Medicine, King George’s Medical University, UP, Lucknow
3Department of Physiology, King George’s Medical University, UP, Lucknow
4Department of Respiratory Medicine, King George’s Medical University, UP, Lucknow
*Correspondence: Dr. Surya Kant, Professor and Head, Department of Respiratory Medicine, King George’s Medical University (KGMU), UP, Lucknow. Email: skantpulmed@gmail.com. Tel: 9415016858.
Abstract
Tuberculosis (TB) is a major global health problem and may appear as a multisystem disease. The two types of clinical manifestation of tuberculosis (TB) are pulmonary TB (PTB) and extrapulmonary TB (EPTB). The former is most common. Extrapulmonary tuberculosis (EPTB) elaborates the diverse situations caused by Mycobacterium tuberculosis (Mtb) infection of tissues or organs exterior the lungs. There are abundant forms of EPTB, influencing each organ complex in the body. TB is a incorrigible infectious granulomatous disease. The etiologic factor of tuberculosis is Mtb. Mtb bacillus is resistant to acid-fast stain that is disseminate chiefly through the respiratory pathway through assimilation of infected airborne droplets consisting the bacillus, Mtb. Subordinate usually, TB is determinant by revelation to Mycobacterium bovis through consumption of infected, unpasteurized, cow’s milk or different atypical mycobacteria.
Key message: Tuberculosis is chronic granulomatous Disease. It is of two types (1) Pulmonary and Extrapulmonary Tuberculosis. Extrapulmonary TB commonly involves pleura, lymph nodes, gastrointestinal organs, bones and joints, central nervous system (CNS), and genitourinary organs while a rare form of EPTB involve orbit, oral cavity, maxilla, mandible, Tonsil, and Breast. The diagnosis and treatment of EPTB are done as per Revised National Control Program (RNTCP) guidelines.
Keywords: Extrapulmonary tuberculosis, Mycobacterium tuberculosis, Acid-fast bacillus, Anti tubercular therapy
Introduction
Tuberculosis (TB) is a major global health problem and may appear as a multisystem disease [1]. It is a chronic necrotizing bacterial infection characterized by the presence of granulomatous lesions, caused by the Mycobacterium Tuberculosis complex (MTBC). This includes M. africanum, M. microti, Mtb, and M. bovis. Mtb is responsible for 97–99% of disease development. It is an acid-fast bacillus that is transmitted primarily through the respiratory route through inhalation of infected airborne droplets containing the bacillus, Mtb. Less commonly, TB is caused by exposure to Mycobacterium bovis through ingestion of unpasteurized, infected cow’s milk or other atypical mycobacteria. [2,3,4]
The target organ of Mtb is the bronchopulmonary apparatus, and the head and neck are usually secondary. [3] TB has two sequential processes: infection and active disease. Active disease can develop during any period of life in approximately 10% of the subjects who have been infected with the TB bacillus. The disease may involve any or all organs, but the lungs are the most commonly involved (85%) and 50% of untreated patients die within 5 years after the initial infection [5]
EPTB involvement tends to increase in frequency if the immune system is compromised Mycobacteria invade many organs during primary infection, but these foci remain dormant (without disease development) if the host has an effective immune system. Reactivation is accelerated in patients with latent diseases, under conditions where the immune system is suppressed. The risk of EPTB and mycobacteremia increases with advancing immunosuppression. TB infection of any part of body other than lung parenchyma is defined as EPTB. Atypical presentation, lack of diagnostic resources for procurement of tissue or fluid for diagnosis from inaccessible sites and a poor yield of conventional diagnostic methods lead to considerable delay in making the diagnosis or diagnosis is even missed. [6,7]
Epidemiology
EPTB describes the various conditions caused by Mtb infection of organs or tissues outside the lungs. There are numerous forms of EPTB, influencing every organ system in the body. The most commonly affected sites of EPTB are pleura, lymph nodes, gastrointestinal organs, bones and joints, central nervous system (CNS), and genitourinary organs.[8] Other rare forms of EPTB includes orbit, oral cavity, mandible, tonsils, maxilla, breast etc (Table 1) .[9,10,11,12,13,14]
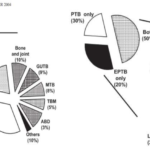
The percentage of EPTB among all TB cases in developed countries ranges from 12 to 28.5%. In developing countries like India, the percentage of EPTB cases is between 15- 20% which has increased to more than 50% among HIV co-infected patients (Figure 1).[2]
EPTB is a less virulent disease in comparison to pulmonary tuberculosis in the form of infectivity. There is paucibacillary load in EPTB. Rising trend of HIV infection has given special attention to EPTB. HIV infected patients have higher prevalence of EPTB ranging from 50 -70%. [15]
Prevalence of Different Types of EPTB [15]
Figure 1. Left: HIV negative patients. Right: HIV positive patients.
Types of Extrapulmonary Tuberculosis
EPTB appertain to TB including organs apart from the lungs (e.g., pleura, lymph nodes, abdomen, joints and bones, genitourinary tract, skin and meninges).A subject with both EPTB and pulmonary is assorted as a case of PTB. Alternatively, tuberculous pleural effusion or tuberculous intrathoracic lymphadenitis (mediastinal and/or hilar) without radiographic peculiarity in the lungs, comprises a case of EPTB.[16]
Table. 1 Site, Prevalence and Pathogenesis of EPTB [17]
| Site | Prevalence | Pathogenesis | Treatment |
|
Lymph node tuberculosis (King’s Evil) |
35-50% | M. tuberculosis gains entry into the body via the respiratory tract and undergoes haematogenous and lymphatic dissemination. Hilar and mediastinal lymph nodes are initially involved. | ATT standard first-line regimen is recommended for peripheral lymph node TB. |
| Pleural Effusion and Empyema | 20% | Small subpleural focus ruptures into the pleural space, setting up an interaction between the tubercle bacilli or their specific components inducing a delayed hypersensitivity reaction. | ATT standard First line regimen is recommended. Steroids are not routinely recommended in pleural TB |
| Abdominal Tuberculosis | 3% | Peritoneum, omentum, mesentery and its nodes and other solid intra-abdominal organs such as liver, spleen and pancreas. | Six-month ATT standard first-line regimen is recommended for abdominal TB |
| Neurological tuberculosis | 3% | meningitis (TBM), tuberculoma, and arachnoiditis three form of neurological tb | TB meningitis should be treated with standard first-line ATT for at least nine months |
| Pericardial Tuberculosis | 1% | Pericardial involvement most commonly results from direct extension of infection from adjacent mediastinal lymph nodes, or through lympho- haematogenous route from a focus elsewhere. | Six-month ATT standard first-line regimen is recommended |
| Bone and Joint tuberculosis | 10% commonly spine and hip joint | The infection begins in the cancellous area of vertebral body commonly in epiphyseal location and less commonly in the central or anterior area of vertebral body | Six-month ATT standard first-line regimen is recommended |
| Genitourinary tuberculosis | 3-4% | Haematogenous dissemination from an active site of infection results in GUTB. Initially metastatic lesions (tubercles) are formed in the kidneys. | Six-month ATT standard first-line regimen is recommended |
| Cutaneous Tuberculosis | 2.5 % | In those not previously exposed to M. tuberculosis, miliary tuberculosis of the skin and tuberculosis chancre have been described. Previously sensitized hosts develop lupus vulgaris, scrofuloderma, tuberculosis verrucosa cutis | Six-month ATT standard first-line regimen is recommended |
| oral tuberculosis | <5% | Either due to infected sputum or due to hematogenous spread | Six-month ATT standard first-line regimen is recommended |
| Otorhinolaryngology | <5% | Tuberculosis of the ear develops when the bacilli invade the eustachian tube while the infant is being fed, or, by haematogenous spread to the mastoid process. The focus in the middle ear cleft may present as painless otorrhea. | Six-month ATT standard first-line regimen is recommended |
| Breast Tuberculosis | 1-2% | Primary tuberculosis mastitis is occurred due to direct inoculation of the breast by M. tuberculosis through skin abrasions or duct openings in the nipple. Secondary involvement of breast through lymphatic haematogenous routes, or by contiguous spread from the ribs, pleural space. | Six-month ATT standard first-line regimen is recommended |
Fig. 2 Diagnostic algorithm for extra pulmonary TB.
A definitive diagnosis of TB can be made by culturing Mtb organisms from a specimen obtained from the patient. Drug susceptibility testing (DST) should be performed on the first isolate of Mtb from all patients. Molecular tests are useful in some form of EPTB (Figure 3).
Table. 2 Different Sites of Extrapulmonary Tuberculosis and Suggested Investigations
| Site of extra-pulmonary tuberculosis | Investigations |
| Node (excluding abdominal) | FNAC, LN biopsy, AFB smear, culture and histology, molecular tests |
| Intra-abdominal (excluding renal) | FNAC, Biopsy, Excision and culture, Guided procedures, molecular tests |
| Pleural | Pleural aspirate, AFB smear, |
| total lymphocyte count and differential, biochemistry, Culture, Biopsy and HPE, molecular tests | |
| Renal/urinary tract | Urine for AFB smear &culture |
| Biopsy and HPE, molecular tests | |
| Tuberculous meningitis | CSF – AFB smear, |
| total lymphocyte count and differential, Culture and biochemistry, molecular tests | |
| Bone/joint | Tissue and / or synovial biopsy, and histology, molecular tests |
| Pericarditis | Pericardial aspirate, AFB smear, total lymphocyte count and differential, biochemistry, Culture, Biopsy and HPE, molecular tests |
| Cold Abscess anywhere | Pus AFB smear and culture |
| Tissue biopsy, and histology and culture, molecular tests | |
| Oral cavity | AFB smear and culture, Tissue Biopsy and histology and culture, Molecular Test |
Fig. 3 Different Diagnostic Methods
Histopathology
On histopathological examination, section revealed groups of Langhan’s type of giant cells with peripherally arranged nuclei. Epithelioid cells are distributed throughout the stroma with lymphocytic infiltration (Figure 4).[18]
Fig. 4 Histopathology of oral lesions showing a presence of granulation tissue surrounded by epithelioid cells (black arrow).
Treatment
EPTB remains a significant cause of morbidity and mortality. Thus, early diagnosis and initiation of appropriate treatment are important for reducing morbidity and mortality in patients with EPTB, 6 months of standard anti-TB medical therapy is generally considered appropriate for most forms of EPTB, longer treatment is recommended for TB meningitis and for bone and joint TB. In case of bone and joint TB, few guidelines recommend 6 months regimens, because these customarily achieve microbiologic and clinical cure. Corticosteroids frequently have been used as an adjunctive in the treatment of EPTB.
Capability of computerized tomographic scan, magnetic resonance imaging, endoscopy, laparoscopy, has staggeringly aids in anatomical restrain of EPTB. The disease generally responds to excellence treatment of anti-tuberculosis drug. Biopsy and/or surgery are mandatory to acquire samples of tissue for detection and for treating complications. Further research is required for evolving the most suitable treatment regimens, optimal duration of treatment and safety when used with highly active antiretroviral treatment (HAART) [5,16,17]
Treatment of Tuberculosis- 6 months of standard anti-TB medical therapy is generally considered adequate for most forms of EPTB, longer treatment is suggested for TB meningitis and for bone and joint TB. The two most widely used TB drugs such as rifampicin and isoniazid cannot respond their efficacy against Multidrug-resistant tuberculosis (MDR-TB).
Anti-TB drugs- Recent guideline recommends the same regimen for EPTB as well as PTB. According to RNTCP Guidelines in Category 1 includes Rifampcin, Isoniazid, Pyrazinamide, Ethambutol drugs. Category 1 is recommended for all Extrapulmonary tuberculosis cases which are newly diagnosed and in previously treated cases injection Streptomycin added over Category 1 regimen termed as Category 2. Oral tuberculosis cases also treated in a same way. MDR (Multi drug resistant) Extrapulmonary tuberculosis cases have been treated under DOTS (Directly Observed Treatment Short course). Category 4 and 5 are recommended for MDR-Extrapulmonary and XDR-(Extensively Drug Resistant) Extrapulmonary TB cases. [7,16,17]
Discussion
Extra pulmonary involvement can occur in isolation or along with a pulmonary focus as in the case of patients with disseminated tuberculosis (TB). The current human immunodeficiency virus (HIV) and acquired immunodeficiency syndrome (AIDS) pandemic has appeared in changing epidemiology and has once again brought extra pulmonary tuberculosis (EPTB) into focal point. Lymph nodes are the most common site, followed by pleural effusion and virtually every site of the body can be affected such as orbit, oral cavity, mandible, tonsils, maxilla, breast etc. Since the impersonal presentation of EPTB is not typical, tissue samples for the corroboration of diagnostic can occasionally be difficult to secure, and the standard diagnostic techniques have a poor yield, the identification is often delayed.
Even on histological examination, we observe a granulomatous lesion we ought to consider different entities such as sarcoid, Crohn’s disease, foreign body reaction, tertiary syphilis and cat scratch disease. Regardless of the fact that, laboratory investigations have the chief role which provide the definite evidence and confirms the disease. Presence of Acid Fast bacilli in the specimen is the confirmatory diagnosis of tuberculosis or it can also be confirmed by culture of tuberculosis bacilli [29]. Sputum culture and radiographic evidence are different accessory modes of confirmatory diagnosis. A protocol of taking various deeper biopsies can also ultimately make the job easier. Compulsory steps should be followed to rule out systemic TB such as chest x-ray and a Mantoux skin test. Now molecular tests (CBNAAT, LPA) are playing a pivotal role in diagnosis of EPTB such as pleural tubercular meningitis etc. [2,7,18,19,20,21]
Conclusion
EPTB remains a significant cause of morbidity and mortality. Thus, early diagnosis and initiation of appropriate treatment are important for reducing morbidity and mortality in patients with EPTB. Availability of newer molecular test, liquid culture methods, computerized tomography scan, magnetic resonance imaging laparoscopy and endoscopy has tremendously helped in to make diagnosis of EPTB. The disease generally responds to standard anti-tuberculosis drug treatment. Biopsy and/or surgery are needed to procure tissue samples for diagnosis and managing the complications. Supplementary research is recommended for evolving the most competent treatment for EPTB.
Conflict of interest
None
Acknowledgments
None
References
1. World Health Organization. Global Tuberculosis Report 2017. Geneva: World Health Organization. Available from: http://www.who.int/tb/publications/global report/en/2017
2. Velingker A, Lawande D, Dcosta L. Clinico-epidemiological profile of extra pulmonary tuberculosis in Western India. International Journal of Contemporary Medical Research 2018;5(2):B1-B4.)
3. Kamala R, Sinha A, Srivastava A, Srivastava S. Primary tuberculosis of the oral cavity. Indian J Dent Res 2011;22: 835-838.
4. Kolokotronis A, Antoniadis D, Trigonidis G, Papanagiotou P. Oral tuberculosis: Oral Dis 1996; 2:242-243.
5. Haas DW, Des Prez RM: Mycobacterium tuberculosis; in Mandell GL, Bennett JE, Dolin R (eds): Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases, ed 5. New York, Churchill Livingstone, 1995,2213–2243
6. Shafer RW, Edlin BR: Tuberculosis in patients infected with human immunodeficiency virus: perspective on the past decade.Clin Infect Dis 1996;22:683-704
7. Singh P, Kant S, Gaur P, Tripathi A, Pandey S. Extra Pulmonary Tuberculosis: An Overview and Review of Literatur. Int. J. Life. Sci. Scienti. Res., 2018; 4(1):1539-1541. DOI:10.21276/ijlssr.2018.4.1.5
8. Srivastava K, Kant S, Verma AK, Dubey A. Tuberculosis: An Overview, Everyman’s Science , 2012; L; 11-21.
9. Kaur A, Kant S, Bhaskar SK. Periorbital Tuberculosis Orbit,2007;26:39-42.
10. Tripathi A, Deora A, Kant A, Sharma S. Oral manifestations of tuberculosis.Lucknow medical journal 2011;1:42-44.
11. Kant S, Sharma S, Verma SK, Singh R, Isolated tubercular osteomyelitis of the mandible. The Int J of Orthopaedic Surgery.www.IJOS.com.2008; l9;1-4
12. Kant S, Verma SK, Sanjay Isolated Tonsil Tuberculosis. Lung India 2008;25:163-164.
13. Kant S, Srivastava R, Verma A.K., Singh H.P., Singh S, Ranganath TG, Anand S, Maxillary Sinus Tuberculosis: Various Presentations. Indian J Chest Dis Allied Sci 2013; 55:175-177
14. Kant S, Dua R, Goel MM. Bilateral tubercular mastitis. Lung India. 2007:24(3): 90-93.
15. Sharma SK, Mohan A. Extrapulmonary tuberculosis. Indian J Med Res 2004;120:316–53.
16. Lee Jy. Diagnosis and Treatment of Extrapulmonary Tuberculosis. Tuberc Respir Dis 2015;78:47- 55.
17. Sharma SK, Ryan H , Khaparde S, Sachdeva KS, Singh AD ,Mohan A, Sarin R, Paramasivan C et al. Index-TB Guidelines: Guidelines on extrapulmonary tuberculosis for India Indian J Med Res 2017;145:448-463.
18. Verma AK, Prakash V, Upadhyay R, Kant S, Bhatia A. Oral tuberculosis mimicking malignancy. Muller J Med Sci Res 2015;6:95-7.
19. Kapoor S, Gandhi S, Gandhi N, Singh I. Oral manifestations of tuberculosis. CHRISMED J Health Res 2014;1:11-4.
20. Dogra SS, Chander B, Krishna M. Tuberculosis of Oral Cavity: A Series of One Primary and Three Secondary Cases. Indian J Otolaryngol Head Neck Surg 2013; 65:275–279
21. Jain P, Jain I. Oral Manifestations of Tuberculosis: Step towards Early Diagnosis. Journal of Clinical and Diagnostic Research. 2014 Dec, Vol-8(12): ZE18-ZE21
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/