J Med Discov (2018); 3(1):jmd17056; DOI:10.24262/jmd.3.1.17056; Received December 16th, 2017; Revised January 25th, 2018; Accepted February 17th, 2018; Published March, 16th, 2018.
Giant Inflammatory Polyp due to mucosal prolapse
Mustafa Al Gburi1, Alhareth Alsagban1,Nisar Ahmed1,*
1. Department of Gastroenterology, Park Plaza Hospital, Houston, TX 77004 USA
* Correspondence: Dr. Nisar Ahmed, M.D. F.A.C.G. , Chief of Gastroenterology, Park Plaza Hospital, Houston, TX 77004, USA. Email: nisarahmedmd@yahoo.com.
Abstract
We describe an unusual case of a giant inflammatory polyp (GIP) discovered during screening colonoscopy in a patient with chronic lymphocytic leukemia (CLL). The patient had neither a history of inflammatory bowel disease, nor history of previous intestinal surgery. Biopsy and cultures showed no evidence of infection. Complete Blood Count unexpectedly revealed significant lymphocytosis, and subsequent flow cytometry revealed chronic lymphocytic leukemia. The patient was referred to a Hematologist for further evaluation and treatment. This is the first reported case to the best of our knowledge in English Literatures of GIP most likely due to mucosal prolapse syndrome in a patient with chronic lymphocytic leukemia.
Keywords: Giant Inflammatory Polyp, Mucosal Prolapse Syndrome, Chronic Lymphocytic Leukemia, Screening colonoscopy, Solitary Rectal Ulcer Syndrome
Introduction
Inflammatory Polyps, or “Pseudopolyps”, represent inflamed regenerating edematous mucosa with granulation tissue surrounded by ulcerated tissue [1]. The term giant inflammatory polyp is used to describe inflammatory polyp greater than 1.5 cm in any dimension. Although inflammatory polyps are common, GIP are uncommon. Their clinical presentation can be varied, ranging from asymptomatic (with incidental detection on radiological or endoscopic testing), to symptomatic (with rectal bleeding and colonic obstruction). Despite the benign nature of GIP many patients may require surgical resection for bowel obstruction or bleeding [2,4]. Here we report an unusual case of giant inflammatory rectal polyp mimicking adenomatous polyp of the rectum.
Case Report
60-year-oldAfrican American male was referred to us for Colon cancer screening; He stated he saw blood on toilet paper when he “pushed “due to constipation.
This was his first colonoscopy. He has history of Coronary Artery Bypass Graft (CABG) in 2016. He also has hypertension, quit smoking 6 months ago, and quit alcohol 2 years ago. Clearance was given by a Cardiologist for colonoscopy. Physical exam was unremarkable except for CABG scar, rectal exam was positive for palpable mass.
Complete Blood Count showed WBCs of 28,500/ml (4500 to 11000/ml) with 61% lymphocytes (20–40%). Hemoglobin and hematocrit 15.1g/dL (14 to 18 gm/dL) and 45.2% (41 to 50%), Flow Cytometry was consistent with CLL for which he was under the care of hematologist/oncologist. Patient underwent colonoscopy and was found to have large rectal mass. Biopsies revealed that it was a giant inflammatory polyp with no neoplastic features.
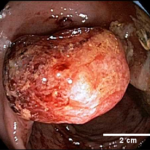
Fig 1. Endoscopic image of rectal mass 5 cm in diameter causing recurrent rectal bleeding.
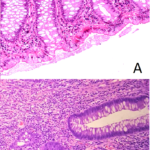
Figure 2.Hematoxylin and eosin staining of normal rectal biopsy in (A) compared to rectal biopsy showing inflammatory polyp with reactive changes, lymphocyte infiltration, but neither dysplastic cells nor malignant lymphocyte found in (B).
Discussion
Our first impression was rectal malignancy either due to suppressed immunity associated with chronic lymphocytic leukemia, or part of malignant infiltration of rectum in CLL. The histopathology confirmed no malignant feature in the rectal mass .So, the most likely etiology in this patient was giant inflammatory polyp due to mucosal prolapse syndrome.
Inflammatory polyps are associated with inflammatory bowel disease, Ischemic colitis, infectious colitis, schistosomiasis, mucosal prolapse syndrome and anastomosis sites. They are benign, although patients with inflammatory polyps due to ulcerative colitis have increased risk of dysplasia .Differential diagnosis includes pyogenic granuloma and vascular tumors such as bacillary angiomatosis and Kaposi sarcoma [1].Inflammatory polyps greater than 1.5 cm in diameter are called giant inflammatory polyps (GIP). Giant Inflammatory polyps can be asymptomatic but most commonly present with abdominal pain, diarrhea, rectal bleeding, or palpable abdominal mass. Other reported manifestations include partial or complete obstruction, protein losing enteropathy, anemia, and intussusception [4-5]. Radiologically and endoscopically, they can be confused with colon cancer. GIP are very rarely caused by Mucosal prolapse syndrome, if so, they are usually located in the rectosigmoid colon and resemble hemorrhoids [3].
Mucosal prolapse syndrome can have multiple and variable expressions with mucosal prolapse as the underlying pathogenic mechanism. The underlying etiology and pathogenesis have not been fully understood but multiple factors may be involved. The most accepted theories are related to direct trauma or local ischemia as causes [6].
Mucosal prolapse syndrome comprises of a variety of clinical and histopathological entities .Disorders considered part of this condition include rectal prolapse, solitary rectal ulcer syndrome (SRUS), proctitiscysticaprofunda (PCP), inflammatory cloacogenic polyp, inflammatory cap polyps and inflammatory myoglandular polyps [6].
SRUS is the most common type of mucosal prolapse syndrome .Clinically, patients often present with passage of mucus or blood per rectum on defecation. In addition, they may report tenesmus , straining, altered bowel habits, partial incontinence and a sensation of incomplete emptying, but patients may also be asymptomatic [6-7].Endoscopically , SRUS can appear as shallow ulcerating lesions on a hyperemic surrounding mucosa, but also as multiple ulcerative lesions, patchy erythematous normal mucosa or as a polypoid lesion. Frequently, patients with SRUS are initially misdiagnosed clinically and pathologically because SRUS is not necessarily solitary or ulcerated. SRUS presenting with rectal ulcers or hyperemia is often labeled Crohn’s disease or mucosal Ulcerative colitis, and polypoid SRUS is often diagnosed as a neoplastic polyp. [6, 8-10].
Conclusion
GIP are rare, but endoscopic biopsy with careful histological examination is essential for correct diagnosis and to rule out foci of dysplasia. Due to re-epithelialization of the surface of inflammatory polyps over time, surface biopsies may show normal colonic mucosa. Hence, complete removal of isolated giant inflammatory polyps should be performed whenever possible.
In conclusion, GIP of the rectosigmoid colon may be caused by mucosal prolapse syndrome or HPV related disorders [3, 11], but due to malignant transformation potential, they must be treated by endoscopic removal or surgery and followed up routinely with colonoscopic surveillance.
Conflict of interest
None
Acknowledgments
We are highly thankful to William Gilmer MD for his help and support.
References
1. Dunn A. Inflammatory polyp of colon. Pathology Outlines – PathologyOutlines.com. 2017. http://www.pathologyoutlines.com/topic/colontumorinflammatory.html.(c) 2002-2017, PathologyOutlines.com, Inc
2. Syal G. Recurrent Obstructive Giant Inflammatory Polyposis of the Colon. ACG Case Reports Journal. 2016; 3(4):e89.
3. Weisenberg E. Inflammatory cloacogenic polyp. Pathology Outlines – PathologyOutlines.com. 2018. http://www.pathologyoutlines.com/topic/anusinflamcloaco.html.(c) 2002-2017, PathologyOutlines.com, Inc.
4. Bandovic J. Giant inflammatory polyp / polyposis of colon. Pathology Outlines – PathologyOutlines.com. 2017.http://www.pathologyoutlines.com/topic/giantcolontumorinflammatory.html.(c) 2003-2016, PathologyOutlines.com, Inc
5. Bandovic J. Inflammatory polyp of colon secondary to mucosal prolapse. Pathology Outlines – PathologyOutlines.com. 2017. http://www.pathologyoutlines.com/topic/colontumorinflammatorymucosalprolapse.html.(c) 2003-2016, PathologyOutlines.com, Inc.
6. Brosens L A A, Montgomery E A, Bhagavan B S, Offerhaus G J A, and Giardiello F M. Mucosal prolapse syndrome presenting as rectal polyposis. Journal of Clinical Pathology. 2009; 62(11):1034-6.
7. Tendler D. Prolapsing mucosal polyps: an underrecognized form of colonic polyp–a clinicopathological study of 15 cases. The American Journal of Gastroenterology. 2002; 97(2):370-6
8. Zhu Q, Shen R, Qin H, Wang Y. Solitary rectal ulcer syndrome: Clinical features, pathophysiology, diagnosis and treatment strategies. World Journal of Gastroenterology. 2014; 20(3):738-44.
9. Gonzalez R. Solitary rectal ulcer syndrome. Pathology Outlines – PathologyOutlines.com. 2017. http://pathologyoutlines.com/topic/colonsolitaryrectalyulcer.html.
(c) 2003-2017, PathologyOutlines.com, Inc.
10. Abid S, Khawaja A, Bhimani S A, Ahmad Z, Hamid S, and Jafri W. The clinical, endoscopic and histological spectrum of the solitary rectal ulcer syndrome: a single-center experience of 116 cases. BMC Gastroenterology. 2012; 12:72..
11. Libânio D, Meireles C, Afonso L P, Henrique R, Pimentel-Nunes P, and Dinis-Ribeiro M. Mucosal Prolapse Polyp Mimicking Rectal Malignancy: A Case Report. GE Portuguese Journal of Gastroenterology. 2016; 23(4): 214-17.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/