J Sci Discov (2018); 2(1):jsd18002; DOI:10.24262/jsd.2.1.18002; Received October 28th, 2017, Revised January 01st, 2018, Accepted January 19th, 2018, Published January 26th, 2018.
Sister Mary Joseph Nodule, a benign looking sign of underlying malignancy
Omar N. Saab1, Mohanad A. Albayyaa1, Imad Alwahashi1, Muhammad Mehdee1, Nisar Ahmed1*
1Department of Gastroenterology, Park Plaza Hospital, Houston, TX, 77004
* Correspondence: Nisar Ahmed, M.D. F.A.C.G, Chief of Gastroenterology, Park Plaza Hospital, Houston, TX 77004, USA. Email:nisarahmedmd@yahoo.com.
Abstract
Albeit it may look benign, Sister Mary Joseph nodule is a sign of underlying malignancy. It is found to be a metastasis from variety of intra-abdominal and pelvic cancers. It has been suggested that such metastasis occurs through different pathways like peritoneal and lymphatic spread.
Keywords: Sister Mary Joseph Nodule; Umbilicus; Malignant
Introduction
Sister Mary Joseph nodule is a palpable nodule in the umbilical region. Despite its benign appearance, it is a warning sign for a hidden malignancy. It may be the presenting feature of an abdominal or pelvic cancer that can be detected even before the primary cancer is symptomatic.[1] It has been noticed that such primary cancers usually originate from the gastro-intestinal tract. like stomach, colon, and pancreas.[2]
Case Report
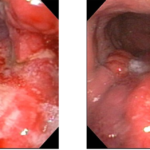
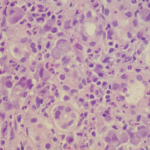
A 60 year old Hispanic female was referred to us with recurrent postprandial right upper abdominal pain, vomiting with black colored stools intermittently for two months. She complained of early satiety and some weight loss. She denied rectal bleeding. She did not smoke or drink alcohol. Past medical and surgical history was significant for a brain tumor treated with surgery, chemotherapy and radiotherapy, more than ten years ago. Her mother died from gastric cancer. Clinical examination showed normal vital signs, the patient was pale, with tenderness in the epigastric and right upper quadrant with no palpable abdominal mass or hepatosplenomegaly. She did have induration and firmness near the umbilicus but no obvious mass. Esophagogastroduodenoscopy showed a large ulcerated, partially circumferential mass with increased friability, in the body of the stomach, (Fig. 1). Biopsies of the mass showed it to be a signet cell adenocarcinoma, (Fig. 2).
Figure 1: Gross appearance by endoscopy
CT scan of the abdomen showed gastric wall thickening with 4.1 x 3.8 cm. Eccentric mass in the greater curvature of the stomach, and mass in the peritoneum and omentum in the area of the umbilicus.
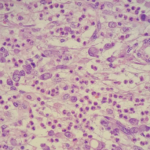
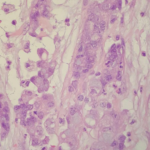
Patient had Gastro-jejunostomy with removal of gastric and umbilical masses. Surgical pathology showed signet cell adenocarcinoma of the stomach and umbilical nodule Fig. 3&4, and the patient sent back to the surgeon for follow up.
Figure. 2: Histological examination of endoscopic biopsy of gastric mass.
Figure. 3: Histological examination of surgical biopsy of the gastric mass.
Figure. 4: Histological examination of surgical biopsy of the umbilical mass
Discussion
Umbilical nodules are classified as being either benign (like congenital polyps) or malignant, primary or secondary lesions. Of all malignant causes, Sister Mary Joseph nodule accounts for 60% and has poor outcome.[2, 3]
Sister Mary Joseph nodule was named after the surgical assistant of Dr. William Mayo, Sister Mary Joseph, in the early days of the Mayo clinic in Rochester, Minnesota, U.S.A.[4] Sister Mary Joseph identified the relationship between umbilical nodules and advanced intra-abdominal malignancies.
It was found that this lesion was a metastatic nodule from variety of underlying cancers. In about third of cases, no primary tumor was detected. However, the culprit lesion was found to originate from carcinomas of stomach (25 %), ovary (12.4 %), colon (10%), and pancreas (7.4%).[2, 5]
The metastasis occurs through direct peritoneal spread or via lymphatic that run beside the obliterated umbilical vein or within remnant falciform ligament, median umbilical ligament or umbilical duct. In some occasions, Sister Mary Joseph nodule can be associated with ascites, cachexia and bleeding per rectum, although no primary tumor was found despite extensive search for the same.[6] The majority of patients with Sister Mary Joseph Nodule have poor prognosis and die within few months after diagnosis.[7]
Conclusion
Sister Mary Joseph nodule is a manifestation of a hidden malignancy and its recognition mandates extensive search for the primary cause. In other words, such finding should not be overlooked.
Conflict of interest
None
Acknowledgments
None
References
1. Sister Mary Joseph nodule-A case report with review of literature Ishrat Hussain Dar, Mqtasid Ahmed Kamili, Showkat Hussain Dar, Faiz Ahmed Kuchaai J Res Med Sci. 2009 Nov-Dec; 14(6): 385–387.
2. Barrow MV (1966) Metastatic tumours of the umbilicus. J Chronic Dis 19:1113–1117
3. Touraud JP, Lentz N, Dutronc Y, Mercier E, Sagot P, Lambert D (2000) Umbilical cutaneous metastasis (or Sister Mary Joseph’s nodule) disclosing an ovarian adenocarcinoma. Gynecol Obstet Fertil 28:719–721
4. H. Bailey: Demonstration of physical signs in clinical surgery. 11th edition, Baltimore, Williams & Wilkins, 1949, p 227
5. Larentzakis A, Theodorou D, Fili K, Manataki A, Bizimi V, Tibishrani M, et al. Sister Mary Joseph’s nodule: three case reports. Cases Journal. 2008; 1:182.
6. Sister Mary Joseph nodule of the umbilicus Author: Dr John Adams, Dermatologist, Wellington, 2008.
7. Abu-Hilal M, Newman JS. Sister Mary Joseph and her nodule: Historical and clinical perspective. The American Journal of the Medical Sciences 2009; 337: 271-273.
Copyright
© This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/